> Abstract
A diagnostic dilemma commonly encountered by the clinician is whether the abnormal gait of a dog can be attributed to a neurological or an orthopaedic origin. In general, lameness is considered to result from orthopaedic disorders, whereas ataxia is expected to be neurological in origin. However, it is not uncommon to encounter cases with uncoordinated gait due to orthopaedic disorders (e.g. hip dysplasia) or lameness due to neurological disorders (e.g. nerve root signature). In order to solve this diagnostic riddle, the careful collection of data from the physical examination and, especially, from the orthopaedic and neurological examination, as well as from several diagnostic tests including imaging and electrophysiology testing are necessary.
> Introduction
Diagnosing the cause of the mobility disorders of an animal can be difficult, a fact which is fairly common in mild disorders or disorders including multiple limbs. Usually lameness is observed in orthopaedic conditions and paresis and/or ataxia in neurological disorders, although the opposite can also be observed. Taking a thorough history and performing a physical examination with emphasis in the orthopaedic and neurological evaluation, will provide the clinicians the necessary information so that they may reach the correct diagnosis.1
> Memorandum
Gait. Each step includes a stance phase, during which the limb rests on the ground, and a swing phase, during which the limb is not on the ground but ambulates forward, with the latter being briefer than the former. When speed increases (trot, gallop) the swing phase increases in duration, whereas the weight bearing phase becomes briefer. Step width is the distance between two consecutive contacts of the limb on the ground.2
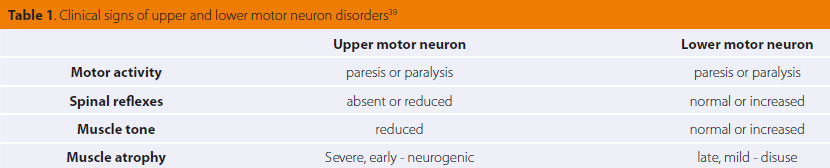
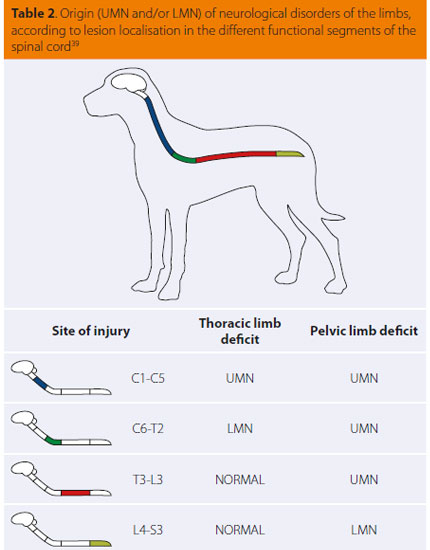
Upper motor neurons (UMΝ). These are efferent neurons that connect the cerebral cortex with the lower motor neurons and modify the activity of the latter. They contribute in starting and preserving motion and provide muscle tone to the extensor weight-bearing muscles against the effect of gravity. They have a suppressing effect on the deep tendon reflexes3 (Τables 1 & 2).
Lower motor neurons (LMΝ). They connect the UMN with the corresponding functioning organs e.g. the skeletal muscles. Essentially these are the nerves. They have a stimulating effect on the deep tendon reflexes3 (Tables 1 & 2).
Animals presenting with lameness tend to reduce the stance phase during the gait cycle so as to reduce the duration of weight-bearing on the affected limb. The opposite is noted on the contralateral healthy limb. Lameness is characteristic of musculoskeletal disorders (bones, joints, tendons, muscles) causing pain and/or mechanical dysfunction of the limb. It is rarely observed in disorders of the nervous system.4
 |
|
(C= cervical, T= thoracic, L= lumbar, |
P a r e s i s is defined as the reduced weight-bearing ability and/or the inability to consciously begin and complete the step cycle. The total inability for conscious movement (e.g. performing the gait cycle) is called p a r a l y s i s and it is physically distinct. When the aforementioned neurological signs affect a single limb this is called monoparesis or monoplegia, respectively. In paretic animals, the step width varies.5 Therefore, when paresis is caused by UMN damage there is a delay in initiating the swing phase, and step width increases. Furthermore, an increase in extensor muscle tone can be observed (spastic paresis). It is worthy of note that in case of UMN paresis, simultaneous ataxia is usually observed (see below). On the contrary, in cases of LMN paresis step width decreases, and in more severe cases the limb may be unable to support the corresponding weight (flaccid paresis). Similar clinical signs are present in muscle and neuromuscular junction disorders.6
A t a x i a is the absence of gait coordination and it can be caused by loss of proprioception (proprioceptive ataxia). It originates in conscious proprioceptive pathways and results in uncoordinated gait, with an increase of the distance between contralateral limbs (abduction), therefore resulting in giving the impression of a swinging motion in the trunk. Furthermore, the animal may walk supporting its weight on the dorsal aspect of the toes.7 An increase in duration of the swing phase may be evident (hypermetria), or a decrease (hypometria) or the presence of both signs (dysmetria). When the vestibular system is unilaterally affected, a head tilt is noted (vestibular ataxia). Τhe animal may suffer loss of balance or even roll around its horizontal axis toward the side of the head tilt. During bilateral vestibular syndrome the head tilt may be absent.8 Finally, during cerebellar ataxia the limbs are abducted with uncoordinated range of motion and the presence of hypermetria is common without simultaneous loss of proprioception. Intention tremors of the head can also be noted.7
>Diagnostic investigation
History and physical examination
In order to diagnose a case with mobility disorders, one begins by obtaining a history and performing a physical examination. Components from the signalment, such as age and breed, may be significant in the diagnostic approach. In particular, several orthopaedic conditions, such as osteochondritis dissecans, are encountered in young animals, as opposed to bone tumours or cranial cruciate ligament rupture, which are more often encountered in middle aged or older dogs.9 Also, adults from chondrodystrophic breeds such as French Bulldog and Pekingese dogs, usually suffer from Hansen type Ι intervertebral disk disease in the cervical and thoracolumbar spine.1 Labrador retrievers are more likely to present with elbow dysplasia compared to other canine breeds.10 Other necessary information that must be derived from the owner includes how the mobility disorder initially emerged, whether it was connected to a traumatic event, its duration, any possible deterioration, any previous treatment regimens and their result, as well as the presence of clinical signs from other organ systems. Examples of musculoskeletal lameness include any disorders of the foot pads, during which extensive licking of the affected areas is reported and lameness is present while walking on rough surfaces.1
The physical examination should begin by obtaining the temperature and it should be detailed, so that any conditions non-related to ambulatory abnormalities can be detected. Pyometra is included in disorders in which lameness can develop, although aetiopathogenesis has not been clarified. Possible causes include several immune mechanisms, endotoxins, severe abdominal pain or even pressure exerted by the distended uterus to the peripheral nerves and corresponding muscles.11
Orthopaedic examination
Τhe animal is observed during standing, walking and trotting. This evaluation aids in investigating orthopaedic, as well as neurological disorders.12 Τhe animal is then guided across both a horizontal and an inclined, non slippery ground. Observing the animal during ascending and descending steps should not be overlooked, especially when the presence of neurological damage is being estimated.13 Τhe gait should be assessed while the animal is walking towards and away from the clinician. Furthermore, overall movement should be observed from the side, and when the dog cannot support its weight, it is necessary to offer assistance so that the ability to move the limbs and coordinate movement can be assessed.14 One more critical point is the evaluation of even weight-bearing while walking. Usually, 60% of the total weight is supported by the thoracic limbs, whereas in some cases this distribution can change. A characteristic example is rupture of ligaments on the caudal surface of the carpi, in which carpal hyperextension leads to increased weight being redistributed to the pelvic limbs.13 During standing, there is usually an attempt to keep the affected limb abducted so as to reduce weight-bearing. In contrast to dogs, cats may conceal lameness or be unwilling to move. In order to verify the presence of lameness, they are released for a longer period of time inside the examination room, in order to adjust to their surroundings. They are placed far away from the spot where they may attempt to hide, so as to be forced to move towards it, while the clinician stands outside the examination room and observes the cat through the window of the closed door. Finally, the owner may bring a video which shows the cat moving in its home.12
A mild lameness may become apparent only during fast movement, whereas some animals may adopt a particular gait, during which they move ipsilateral limbs simultaneously. While this gait may be normal in some large animals, it may also indicate osteoarthritis because in this way overextension of the joints can be avoided. In cases of thoracic limb lameness, animals elevate their head when weight is supported on the affected limb, and lower it when the weight shifts to the contralateral healthy limb. Simultaneous to head lifting there is contralateral shoulder dropping.10 In cases of hind limb lameness, head lowering and extension of the neck is noted in an effort to transport weight toward the front limbs. When the affected pelvic limb is placed on the ground, the head and neck downward movement may intensify in order to further reduce the weight distributed to the pelvic limbs. The movement of the tail is also indicative of lameness of the hind limb. More specifically, as opposed to the horizontal motion observed in normal dogs, it moves downward and up, with the latter noted when the affected hind limb touches the ground. With this motion the weight distributed to that limb is reduced. Simultaneous to tail motions, usually a tilt of the pelvis is noted toward the affected side. Dogs with pelvic limb lameness shift the thoracic limbs caudally, almost completely reducing weight bearing on the affected limb with minimal movement of the head during ambulation.4
Τhe dog is encouraged to sit or recline and then immediately to rise again, because these motions are performed with difficulty in conditions like lumbosacral stenosis and osteoarthritis due to hip dysplasia. In severe orthopaedic conditions simultaneously affecting both hind limbs, walking may not be possible, or steps with smaller width are observed in the affected limbs, resulting in a resemblance to neurological cases.7 Sometimes, when these animals run, the hind limbs are moved simultaneously (bunny hopping), so that weight is evenly distributed in both hind limbs and full extension of the affected joints can be avoided.2 Such disorders include hip dysplasia, patellar luxation, cranial cruciate ligament rupture, and hip and knee osteoarthritis. 8
After observing ambulation, palpating the muscles is necessary. Initially the examination is performed while standing, so that simultaneous palpation of the frontal and then caudal limbs is possible and any asymmetry between the two, mainly due to muscular atrophy, can be detected. This atrophy can result from reduced use of the affected limb or it can be neurogenic and it can also be unilateral or bilateral depending on the initiating cause. Furthermore, oedema and pain of the corresponding muscles can be observed. In this position, the spine and pelvis are examined, with particular attention to the symmetry of the latter.12 Pain during spinal palpation and findings from the neurological examination, that will follow, may guide the clinician towards a motility disorder of neurological origin.1,15 The orthopaedic examination continues with the animal reclining on its side, and it must always begin with the healthy limbs.12 All limbs are examined from the periphery to the center, meaning from the toes to the scapula or pelvis. All the bones are palpated for pain or disfigurement, as well as the joints for possible reduction in range of motion and the presence of pain, oedema, crepitus or instability.1
Neurological examination
The neurological examination is performed initially during the orthopaedic examination, and is completed afterwards. In particular, during orthopaedic examination at a standing position, postural reactions are evaluated to aid in detecting disorders not apparent during walking.16 These include paw placing in abnormal position, wheelbarrowing, hopping, hemiwalking, the extensor postural thrust and tactile and visual placing. During proprioceptive testing the examiner’s hand should support the animal under the chest or pelvis for the thoracic and pelvic limbs, respectively, so that any painful disorders of the limbs will not affect the postural reactions.15 Abnormal responses are indicative of neurological disorders. However, from the evaluation of the proprioceptive responses in a single limb, it is not possible to localise the lesion, because the normal response depends on the correct function of sensory neurons, the spinal cord, the brainstem, the thalamus, the cerebral cortex and the motor neurons.14 In contrast, the evaluation of the proprioceptive responses from all four limbs may offer significant information for lesion localisation. Furthermore, it is important to examine the cranial nerves and the level of consciousness because they may be disrupted by cerebral lesions.7 In cats, performing all these diagnostic procedures is challenging, therefore mostly hopping and wheelbarrowing are performed, as well as gradually sliding the limb laterally, which, in normal cats, will result in an immediatereturn of the paw to the normal standing position.16
The neurological examination is completed by assessing the spinal reflexes, mostly at a lateral recumbency. The most important spinal reflexes include the patellar reflex, the cranial tibial muscle reflex, the sciatic nerve reflex, the extensor carpi radialis muscle reflex, the anal and cutaneous trunci reflexes, as well as the withdrawal reflexes of the thoracic and pelvic limbs.17An abnormal response in the spinal reflexes, especially when it coincides with abnormal proprioception, may indicate lesions in the peripheral nerves, the spinal cord or the neuromuscular synapses.14 When the spinal reflexes are increased, it is indicative of UMN lesions, but when they are reduced or absent, it is indicative of LMN disorders.17 In particular, LMNs comprise the neuronal supply for the limbs, and therefore, their disorders may result in flaccid paresis or paralysis of the limbs and they are commonly associated with orthopaedic conditions. Other characteristic clinical signs for LMN syndrome include hyporeflexia or areflexia in muscles that are innervated by the spinal nerves.15 The latters are detected by palpating the muscles or performing mild flexion and extension of the joints of the affected limbs, because in normal animals there is a slight resistance during this movement. Furthermore, there is severe simultaneous muscle atrophy, which develops faster (in a period of 1 week) than that, due to UMN atrophy or due to inactivity.12 By applying painful stimuli to the toes, deep pain perception is assessed, which is indicative of the severity of the neurological disorder.17 Particular care must be taken so that this test is not confused with the withdrawal reflex, in which the animal merely flexes its limb. When deep pain sensation is present, the dog will bark, try to bite or there may even be mydriasis or increase in heart and respiratory rate. One must be especially careful when musculoskeletal disorders affect the execution of spinal reflexes, e.g. the withdrawal and patellar reflex. Characteristic examples include cranial cruciate ligament, hip dysplasia and myopathies, which may decrease the ability of the animal to fully flex its limb.8 Finally, in cases of nerve compression, such as dorsolateral intervertebral disk disease (IVDD) or the growth of a tumour, the corresponding limb may not bear weight imitating lameness of musculoskeletal origin (nerve root signature).15,16
Other diagnostic examinations/tests
Diagnostic tests that can be used to differentiate orthopaedic from neurological disorders include imaging (standard radiography, myelography, ultrasonography, computed tomography and magnetic resonance imaging), cerebrospinal fluid analysis in order to reveal inflammatory disorders or neoplasms in the central nervous system, synovial fluid analysis,7 and histopathology.1
More specialised diagnostics include electrophysiology testing, because it may confirm whether the motility disorder is a result of neuropathy or myopathy. Electromyography, nerve conduction studies and f-wave study, as well as repetitive nerve stimulation are included in standard electrophysiology testing performed in dogs under general anaesthesia.15 Εlectromyography, in particular, can assess the entire motor unit by recording muscle electrical activity and in particular the neurons of the ventral horn of the spinal cord and their neuraxons, the neuromuscular synapses and the muscle fibers.18
> Neurological or orthopaedic case? Examples
Neurological disorders
In the clinical setting, the most common mobility disorder is caused by herniation of intervertebral disks. Herniation of the nucleus pulposus (Hansen type I IVDD) occurs when the latter undergoes chondroid metaplasia.19 The severity of clinical signs can vary, from mild, with only spinal hyperesthesia, to severe with paraplegia and loss of deep pain sensation.20 This condition is mostly common in chondrodystrophic dog breeds and is usually observed in the cervical and thoracolumbar spine.19 In contrast, herniation of the annulus fibrosus (Hansen type II IVDD) commonly develops after fibrous metaplasia of the nucleus pulposus,21 hyperplasia or hypertrophy of the annulus fibrosus and prolapse of a portion of it in the spinal cord. This results in chronic compression of the spinal cord and demyelination19 and it is usually observed in the caudal cervical, thoracolumbar and lumbar spine.20 Nerve root signature with pain and lameness in a single limb may occur when a single intervertebral disk has compressed a spinal nerve root or is herniated in the spinal cord at the cervical or lumbar spine.15,16 Reaching a diagnosis of IVDD is based on clinical findings and especially on the neurological examination which is characterised by hypersensitivity of the spinal cord. The diagnosis is confirmed by imaging, including computed tomography, myelography and magnetic resonance imaging.15 In particular, in IVDD of the cervical spine, dogs have ataxia and paresis in all four limbs, as well as severe pain during cervical palpation, muscle spasm of the corresponding muscles and abnormal head position. In IVDD in the thoracolumbar spine, hypersensitivity in the area of IVD herniation, and paraparesis or paraplegia can be observed.22
Lumbosacral syndrome is usually manifested in large dog breeds and is one of the most common causes of paresis and/or hindlimb lameness. It is commonly mistaken for hip dysplasia. Usually it is caused from degenerative myelopathy or idiopathic lumbosacral stenosis, fractures or subluxations in the lumbosacral spinal cord, as well as congenital abnormalities in this location. Other causes of this syndrome include diskospondylitis and tumours. Diagnosis is based on clinical findings such as gluteal and popliteus muscle atrophy, a reduced response in positional reflexes and pain during palpation of the lumbosacral spine,23 as well as imaging (standard, myelography), computed tomography and magnetic resonance imaging.24
Tumours of the spinal cord, vertebrae and spinal nerves can be a cause of lameness in animals. In particular, vertebral neoplasms and extradural tumours may compress the spinal nerves (nerve root signature) and result in lameness of the thoracic or pelvic limbs depending on whether the compression is located in the cervical or thoracolumbar spine, respectively.12 The pain caused by these tumours can have phases of exacerbation and remission, whereas in cases where the neoplasm has already been diagnosed, the acute manifestation of severe pain with simultaneous neurological signs is an indication of a pathological vertebral fracture. Diagnosis for vertebral and extradural tumours is obtained via radiographs (standard or during myelography) and computed tomography. In contrast, in order to diagnose intradural neoplasms, myelography, standard radiography, computed tomography or magnetic resonance imaging can be used.25
In the spinal nerves, schwannomas are usually encountered, and they are malignant. They are usually located in the spinal cord, near the spinal nerve roots.12 When they are located inside the vertebral canal, they may compress the spinal cord and, according to which segment is compressed, this can result in the corresponding neurological signs. In the cervical spine they may result in cervical pain and neurological deficits in the affected limb, and, rarely, to the rest of the limbs as well. In the cervicothoracic segment of the spinal cord they may cause Horner’s syndrome and affect superficial sensation. In contrast, schwannomas that compress the lumbosacral spine may lead to neurological deficits only in chronic cases.1 Νeoplasms can occur in the brachial or lumbar plexus and they are manifested by progressive lameness and muscle atrophy of the thoracic or pelvic limbs, respectively. The diagnosis can be reached with palpation of the mass, when the tumour is located outside the spinal cord, with radiographs (standard, myelography), with electrophysiology testing, computed tomography and/or magnetic resonance imaging. In human medicine, in order to diagnose peripheral nerve tumours, ultrasonography is also used.15
Finally, in polyneuropathies, the motility disorder usually initiates from the caudal limbs. With proper support, the dogs respond normally to proprioceptive tests, deep tendon reflexes are absent or reduced and there is no ataxia. The muscles are flaccid and there is neurogenic muscular atrophy.26,27
Οrthopaedic disorders
Ataxia and muscle weakness during walking is mostly observed in neurological disorders. However there are orthopaedic conditions that cause lack of limb coordination and increase in joint flexion and extension range of motion compared to the normal. 1 Moreover, in certain orthopaedic disorders the steps are smaller in width and abnormal placement of the limb on the ground is noted with valgus or varus deviation.2
Thoracic limbs
Muscle weakness during gait assessment observed in the front limbs may result from a dislocated shoulder joint, as well as an olecranial avulsion fracture. Moreover, the avulsion or rupture of the triceps brachii tendon may limit the shoulder joint range of motion.1 During carpal sprains there is ligament injury and severe gait abnormalities are observed. Carpal hyperextension resulting from severed palmar ligaments, is usually caused by fall from a height. When all the carpal ligaments are severed, joint instability is apparent. Diagnosis is based on orthopaedic examination, stress radiography and magnetic resonance imaging. On the other hand, partial palmar ligament rupture cannot be diagnosed with radiography.28 Permanent contracture of the infraspinatus muscle and more rarely, supraspinatus muscle and teres minor muscle injuries, may be initially manifested as thoracic limb lameness during exercise that persists for about two weeks, without necessarily being connected to a previous history of trauma.1 After an intermediate time period of a few weeks with normal motility, an obvious rotatory motion is manifested, as well as jerking movements of abduction and extension of the peripheral part of the limb as it is moved forward. During standing the peripheral part of the limb is abducted and the elbow is adducted. During the orthopaedic examination a reduction in range of motion of the joint is noted, and it is also possible to observe infraspinatus, supraspinatus and teres minor muscle atrophy. This condition resembles suprascapular nerve injury. Diagnosis of this muscle contraction is done by orthopaedic examination, electrophysiology testing, as well as histopathology in order to detect muscle atrophy and fibrosis.29
One more condition, which in severe forms could be mistaken for radial nerve paralysis is contraction of the flexor carpi ulnaris in puppies. During this disorder the carpus is in various degrees of hyperflexion, no pain is evident and the animal can exercise normally. Diagnosis is based on the presence of an increasingly taut flexor carpi ulnaris muscle and the absence of neurological or radiological findings.30
Pelvic limbs
A characteristic example of muscle weakness during walking is manifested in dogs with hip dysplasia. Diagnosis is reached through orthopaedic examination, since the dog usually has a stiff gait which deteriorates with exercise. There is simultaneous pain and crepitus in passive range motion movements of the hip joints, as well as a positive Ortolani sign. Radiography plays an important role in order to reach the diagnosis.31 Furthermore, cranial cruciate ligament rupture can lead to instability of the stifle joint, resulting in the mistaken impression that there is an ataxic gait. The rupture may be diagnosed during orthopaedic examination from the pathognomonic caudal drawer motion of the stifle. Moreover, patellar fractures, rupture/avulsion of the patellar ligament, intratarsal fractures and sprains of the tarsal joint can cause weakness during walking.1 Rupture of the Achilles tendon and gastrocnemius muscle avulsion can result in a dropped hock and plantigrade walking. In such cases, the diagnosis is based on the orthopaedic examination and gastrocnemius tendon function testing, as well as ultrasonography. Permanent contraction of the quadriceps femoris muscle can lead to permanent extension of the knee joint and alterations in gait, whereas permanent contraction of the gracilis or semitendinosus muscle causes tarsal outward rotation and inward rotation of the knee and the peripheral part of the limb.32
Polyarthritis
Polyarthritis can be a cause of abnormal ambulation in animals. Depending on the initiating cause, they can be classified as infectious or immune-mediated. Τhe typical signs include anorexia, lameness or even inability to rise, oedema and pain in the joints, as well as hyperthermia. The most commonly affected joints include the carpi, the knees and the tarsi.33 Immune-mediated, non-ulcerative polyarthritis is the most common type and it is connected with systemic disorders, neoplasms, systemic lupus erythematosus, drug administration (phenobarbital) or it may even be idiopathic. It is noted that dogs of the Αkita breed are predisposed to the disease.34
Myopathies/Synaptopathies
These are congenital or acquired disorders of skeletal muscles or neuromuscular junctions. They are usually symmetrically distributed and some canine breeds are predisposed.35 Specifically, a form of congenital myopathy is noted on the 8th week of life in Labrador Retrievers.36 In these conditions the spinal reflexes and deep pain sensation are usually normal. Usually in myopathies, there is a generalised muscle weakness, which can be connected to inability to exercise, exhaustion and stiff gait. In most cases, muscle weakness deteriorates with exercise. In contrast, in myotonic disorders, such as congenital myotonia, stiffness, which is a characteristic of myopathies in general, tends to improve during exercise. Furthermore, pain is elicited during muscle palpation, whereas localised or generalised muscle atrophy may be simultaneously evident,15 or the affected muscles can be enlarged due to inflammation, contraction or hypertrophy.37 The diagnostic investigation includes evaluating the clinical signs in combination with electrophysiology testing.15 In standard haematology testing, there may be indications of infectious or immune-mediated aetiology, whereas biochemistry may reveal an increase in creatine phosphokinase serum concentration, because it is directly linked to muscle diseases. The definitive diagnosis is reached through histopathologic examination of biopsy samples, which follows after locating the most severely affected muscle groups with electromyography.37,38
> Conclusion
It is common in the clinical setting for the veterinarian to be called upon to decide whether cases of gait abnormalities are neurological or orthopaedic, so that the prognosis and treatment can be defined. In order to solve this problem clues from the signalment, history, and physical, orthopaedic and neurological examination are taken into consideration. Further diagnostics, such as imaging and electrophysiology testing, could aid in this direction.1
> References
1. McKee M. Lameness and weakness in dogs: is it orthopaedic or neurological? In Practice 2007, 29: 434-444.
2. Leach D, Sumner - Smith G, Dagg AI. Diagnosis of lameness in dogs: A preliminary study. Can Vet J 1977, 18: 58-63.
3. Garosi L. The neurological examination. In: BSAVA Manual of Canine and Feline Neurology. Platt SR, Olby NJ (eds). 3rd edn. British Small Animal Veterinary Association, Gloucester, 2004, pp. 1-23.
4. Nunamaker DM, Blauner PD. Normal and abnormal gait In: Textbook of Small Animal Orthopeadics. Newton CD, Nunamaker DM (eds). Lippincott, Philadelphia, 1985, pp. 1083-1095.
5. De Lahunta G. Lower motor neuron: Spinal nerve, general somatic efferent system In: Veterinary Neuroanatomy and Clinical Neurology. 3rd edn. Saunders Elsevier, St. Louis, Missouri, 2009, pp. 77-133.
6. Schatzberg SJ, Kent M, Platt SR. Neurologic examination and neuroanatomic diagnosis In: Veterinary Surgery Small Animal. Tobias KM, Johnston SA (eds). Elsevier Mosby: St Louis, Missouri, 2012, pp. 325-339.
7. Dewey CW, DaCosta RC, Thomas WB. Performing the neurologic examination. In: Practical Guide to Canine and Feline Neurology. Dewey CW, DaCosta RC (eds). 3rd edn. Wiley-Blackwell, Iowa, 2015, pp. 9-28.
8. Parent J. Understanding the neurological exam. In: The North American Veterinary Conference Proceedings - Companion Animals. Orlando Florida, 2002, pp. 448-453.
9. Johnson AL. Fundamentals of orthopedic surgery and fracture management. In: Small Animal Surgery. Fossum TW (ed). 4th edn. Elsevier Mosby, St. Louis, Missouri, 2013, pp. 1033-1044
10. Scott H, Witte P. Investigation of lameness in dogs: Forelimb. In Practice 2011, 33: 20-27.
11. Klainbart S, Ranen E, Glikman G, Kelmer E, Bdolah-Abram T, Aroch I. Hindlimb lameness and gait abnormalities in bitches with pyometra. Vet Rec 2014, 175: 11-15.
12. Renberg WC. Evaluation of a lame patient. Vet Clin North Am Small Anim Pract 2001, 31: 1-15.
13. Artiles A. The ataxic dog - is it neurological or orthopaedic? - part 1. CPDsolutions, 2014, http://vetgrad.com/show10Minute- TopUp.php?type=&Entity=10MinuteTopUps&ID=61 (accessed March 28, 2017).
14. Mariani CL. Is it neuro or ortho? Sorting out lameness, paresis and dogs that won’t get up. In: Conference Proceedings of the Oklahoma Veterinary Medical Association - Companion Animals. Oklahoma, 2013, pp. 102-105.
15. McDonnell JJ, Platt SR, Clayton LA. Neurologic conditions causing lameness in companion animals. Vet Clin North Am Small Anim Pract 2001, 31: 16-53.
16. Garosi L. Neurological lameness in the cat: Common causes and clinical approach. J Feline Med Surg 2012, 14: 85-93.
17. Wheeler JS. Diagnosis of spinal disease in dogs. J Small Anim Pract 1989, 30: 81-91.
18. Steinberg SH. A review of electromyographic and motor nerve conduction velocity techniques. J Am Anim Hosp Assoc 1979, 15: 613-619.
19. Macias C, McKee WM, May C, Innes JF. Thoracolumbar disc disease in large dogs: A study of 99 cases. J Small Anim Pract 2002, 43: 439-446.
20. Levine JM, Fosgate GT, Chen AV, Rushing CR, Nghiem PP, Platt SR, Bagkey RS, Kent M, Hicks DG, Young BD, Schatzberg SJ. Magnetic resonance imaging in dogs with neurologic impairmet due to acute thoracic and lumbar intervertebral disk herniation. J Vet Intern Med 2009,23: 1220-1226.
21. Smolders LA, Niklas B, Grinwis GCM, Hagman R, Lagerstedt A, Hazewinkel HAW, Tryfonidou MA, Meij BP. Intervertebral disc degeneration in the dog. Part 2: Chondrodystrophic and nonchondrodystrophic breeds. Vet J 2013, 195: 292-299.
22. Garosi L. Lesion localization and differential diagnosis. In: BSAVA Manual of Canine and Feline Neurology. Platt SR, Olby NJ (eds). 3rd edn. British Small Animal Veterinary Association, Gloucester, 2004, pp. 24-34.
23. Palmer RH, Chambers JN. Canine lumbosacral diseases. Part 1. Anatomy, pathophysiology and clinical presentation. Compend Contin Educ Pract Vet 1991, 13: 61-68.
24. Palmer RH, Chambers JN. Canine lumbosacral diseases. Part 2. Definitive diagnosis, treatment and prognosis. Compend Contin Educ Pract Vet 1991, 13: 213-221.
25. Raw ME. The differential diagnosis of cervical pain in the dog. Can Vet J 1987, 27: 312-318.
26. Cuddon PA. Acquired canine peripheral neuropathies. Vet Clin North Am Small Anim Pract 2002, 32: 207-248.
27. Fitzmaurice SN. LMN paresis and paralysis: acquired myasthenia gravis. In: Saunders Solutions in Veterinary Practice: Small Animal Neurology. Saunders Elsevier, London, 2010, pp.186-193.
28. Nordberg CC, Johnson AK. Magnetic resonance imaging of normal canine carpal ligaments. Vet Radiol Ultrasound 1998, 39: 128-136.
29. Whitney DD, Hess JL. Contracture of the infraspinatus muscle in the dog. Iowa State University Veterinarian 1979, 41: 76-80.
30. Holland CT. Carpal hyperflexion in a growing dog following neural injury to the distal brachium. J Small Anim Pract 2005, 46: 22-26.
31. Fries CL, Remedios AM. The pathogenesis and diagnosis of canine hip dysplasia: A review. Can Vet J 1995, 36: 494-502.
32. Moores A. Muscle and tendon disorders in small animals 2. Conditions affecting the hindlimb and digital flexor tendons. In Practice 2012, 34: 74-77.
33. Jacques D, Cauzinille L, Bouvy B, Dupre G. A retrospective study of 40 dogs with polyarthritis. Vet Surg 2002, 31: 428-434.
34. Stull JW, Evason M, Carr AP, Waldner C. Canine immunemediated polyarthritis: Clinical and ladoratory findings in 83 cases in western Canada (1991- 2001). Can Vet J 2008, 49: 1195-1203.
35. Braund KG. Clinical neurology in small animals: localization, diagnosis and treatment. IVIS 2005, http://docs16.chomikuj. pl/3758152435,PL,0,0,clinical-neurology-in-small-animals- Braund.pdf (accessed March 28, 2017).
36. McKerrell RE, Braund KG. Hereditary myopathy in Labrador Retrievers: A morphologic study. Vet Pathol 1986, 23: 411-417.
37. Platt SR, Garosi LS. Neuromuscular weakness and collapse. Vet Clin North Am Small Anim Pract 2004, 34: 1281-1305.
38. Gaschen F, Jaggy A, Jones B. Congenital diseases of feline muscle and neuromuscular junction. J Feline Med Surg 2004, 6: 355-366.
39. Sharp NJH, Wheeler SJ. Patient examination. In: Small Animal Spinal Disorders. 2nd ed. Elsevier, London, 2005, pp. 19-33.



