> Abstract
Fractures of the mandible in cats often occur due to falls from heights, car accidents or human abuse. The current retrospective study describes 23 cases of feline mandibular fractures, which were treated at the Companion Animal Clinic, at the School of Veterinary Medicine of the Aristotle University of Thessaloniki, during 2008-2015. Young male animals were mostly affected. Eight fractures were caused by car accidents, one after falling from great height, one by human abuse and thirteen were of unknown cause. However, thirty-three fractures are discussed in total, as four cats exhibited multiple fractures. In particular, eleven fractures were located in the mandibular symphysis, seventeen in the rammus and five in the body of the mandible. Mandibular symphyseal separation was treated either with metal wire introduced circumferentially behind the canines or with a figure-of-eight wire placed intraorally between the canines, bonded with acrylic resin. Fractures of the body were repaired with wire, placed either interdentally reinforced with acrylic resin or intrabony combined with screws. Eighteen animals were hospitalised postoperatively. Finally, repetitive surgery was required in one case, while recovery was uncomplicated or minimally complicated for the rest.
> Introduction
Fractures of the mandible usually occur in young animals, representing 15-16% of all kinds of fractures in cats and comprising the third most common type of fracture.1-6 Symphyseal separations account for 73% of all fracture types, caused by falls from heights or car accidents.1,2,4-8 Fractures of the body rank second in terms of frequency, followed by intra- or extra- articular fractures of the ramus. Such fractures occur as a result of trauma, such as falls from heights, vehicular accidents or human or animal violence. However, periodontitis, neoplasia, osteomyelitis or serious endocrine disorders can result in pathological fractures.1,2,4-6,9
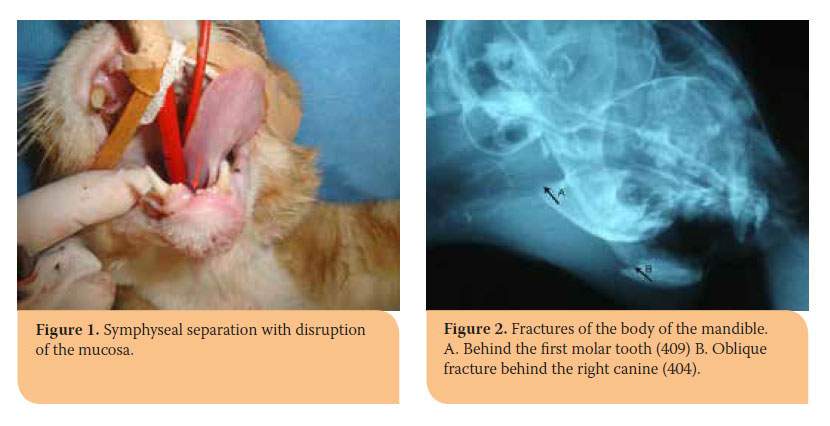
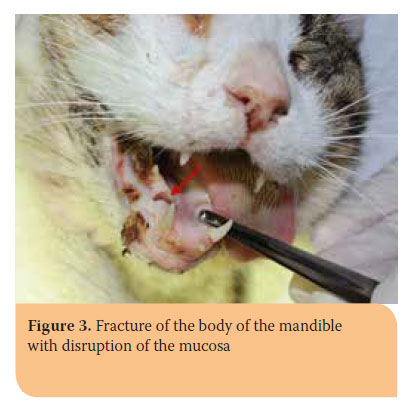
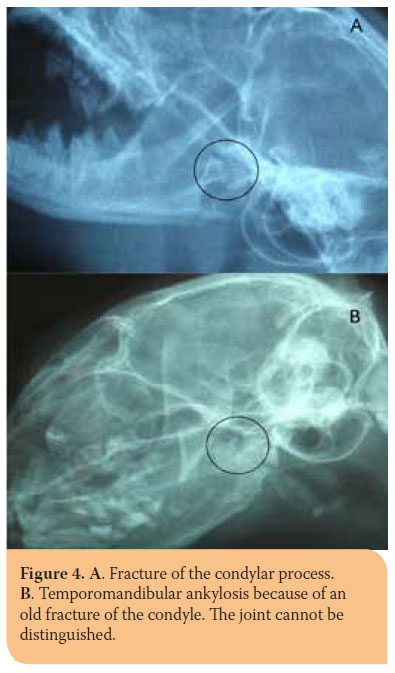
Clinical symptoms depend on the location and extent of the trauma. In most cases pain, abnormal movement, crepitus and teeth malocclusion are found. Moreover, salivation, haemorrhage, nose bleeding, dysphagia or anorexia, injuries of the oral mucosa around the fracture area, etc. may also be exhibited.1,7,10 Symphyseal separations are accompanied by free movement of the hemimandibles, when manipulated, and pain without crepitus (Picture 1).10 Fractures of the body can be located on the molar-, premolar or incisor area of the mandible. Fracture displacement depends on the line of the fracture (Pictures 2,3).5 Clinical diagnosis of subcondylar, condylar or other fractures involving the ramus, can be challenging due to extended coverage by the muscles of mastication.6 Depending on the time elapsed since the incidence, the animal might experience partial or total inability to open its mouth, because of temporomandibular joint ankylosis (Picture 4). Occasionally, fractures of the ramus are accompanied by other types of fractures of the mandible, especially of the symphysis.1,5,11,12
As a result of the animal’s size and the fact that the majority of fractures are of traumatic origin, they may be accompanied by conditions threatening the animal’s life, such as obstruction of the upper respiratory system, pneumothorax, hemothorax, diaphragmatic hernia, pulmonary contusion, internal haemmorhage, shock, trauma of the central nervous system, etc. It is obvious that in case of life threatening traumas, they should be addressed first.1,5,10,11 When repair of mandibular fractures needs to be postponed, the clinician should accommodate for adequate feeding via nasoesophageal or esophagostomy tubes.1,10
Therapeutic intervention should be aimed at repairing the fracture and restoring the normal movement of the jaws. It is imperative to ensure normal occlusion.1,6,9,13 Lower canines are normally located rostral to the upper canines, while the premolars of the upper jaw overlap that of the lower.5,14,15 In order to ensure proper reconstruction, especially when numerous or comminuted fractures are involved, the endotracheal tube should be placed through pharyngostomy.1,3-5,9,16
The most common techniques for mandibular fracture repair are discussed in the current study.
Separations of the symphysis are usually repaired using a circumferential orthopaedic wire just distal to the mandibular canines. A skin incision is performed in the ventral midline and the wire is guided around the lateral borders of the mandible with a pair of hypodermic needles (16 or 18G), exiting through the oral mucosa caudal to the mandibular canines. The wire is tightened with pliers and the knot is buried under the skin (Picture 5). This technique can be also performed with one needle which is introduced laterally to the hemimandible and after the wire is inserted through it, the needle is retracted and reinserted laterally to the other hemimandible through the mucosa from the same skin incision. 1,5,6,8,10,11 Alternatively, when there is bone loss in the symphysis or tooth mobility, a wire in a figure-of-8 is placed around the mandibular canines, and is stabilized with acrylic resin. The latter technique can ensure stability and proper occlusion, as with the former one the surgeon cannot properly control the degree of twisting.1,4,6,7 In order to prevent wire displacement, a small amount of resin is attached to the lateral aspect of the canines before placing the wire, which is then stabilised with an additional amount of acrylic resin (Picture 6). Proper alignment of the canine teeth should be checked before the end of the surgery.1

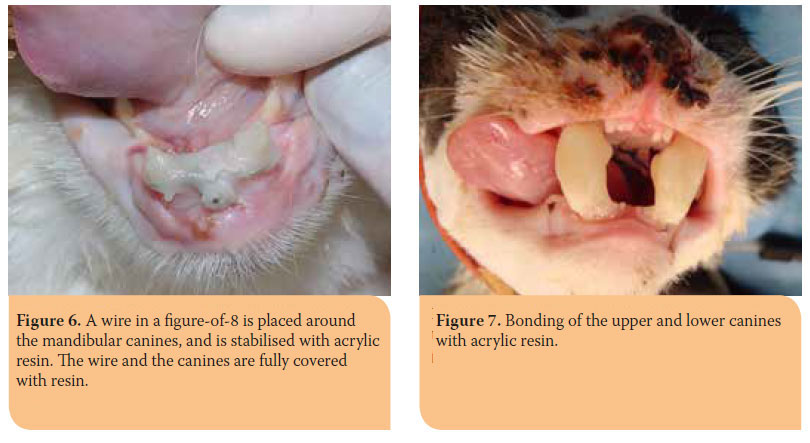
Fractures of the ramus are very difficult to stabilise. It is practically impossible to use osteosynthesis materials because of the size of the bone, especially the size of the condyloid process, which is most commonly affected, as the area is extensively covered with muscles.2,6 Early diagnosis determines the therapeutic modality of treatment.17 In case the fracture remains undiagnosed, callus formation in the temporomadibular joint causes gradual limitation of movement of the mandible and finally ankylosis 4-6 weeks after trauma.1,5,11,12,17.
On condition that the fracture is diagnosed immediately, the treatment of choice is bonding of the upper and lower canines together with acrylic resin for 6 weeks. This modality of treatment favours the formation of a normal-sized callous. When bonding the canines, a 1 cm space should be left between them so that the animal can receive water and soft or liquid food (Picture 7).1,3,6,8,10
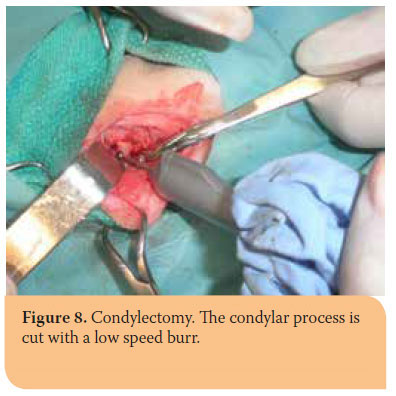
When ankylosis has already occurred at the time of admission, condylectomy, sometimes bilateral, is the only acceptable treatment (Picture 8)1,4,5,11,12 Tracheostomy should be routinely performed prior to surgery for safer anesthesia.12
Fractures of the body can be treated with various methods, such as intraosseous wiring, miniplates, interdental wiring with acrylic resin or external fixation.1,4-6,10,11 Interdental wiring with acrylic resin is a cost-effective method of treatment. However, an adequate number of periodontally healthy teeth should exist on both sides of the fracture line.1,3,5,6,8,10,13,18,19 Moreover, intraosseous wiring is most commonly utilised when fractures in the premolar or molar area are encountered.1,4-6,10 This particular technique assures adequate stability in simple fractures without major displacement or bone loss.1,20 It should be avoided in animals with primary or mixed dentition, because permanent teeth can be easily injured, while it should be cautiously performed in small-sized cats.21 Attention should be also paid not to traumatise the roots of the teeth, the vessels and nerves of the mandibular canal.1,20
Finally, when multiple fractures are encountered in both mandibles, bonding together the upper and lower canines can be used as an ancillary or sole method of treatment, as it has already been described for condylar fractures.13
Teeth usually exist in the fracture line. These teeth should be extracted only if they are severely affected by periodontal disease, have fractured roots or are unstable because they interfere with bone healing. 1,4,5,8-10,22 Stable teeth with fractured crowns are retained, while other with pulp exposure should be endodontically treated.4,5,8-10,22 The aforementioned teeth contribute to the fracture stability and are sometimes involved in the treatment plan , so it is important to be retained.1,4,5,9,10,15
Animals with mandibular fractures occasionally need hospitalization, especially if they have experienced multiple fractures or the canines have been bonded. Especially cats with concomitant facial trauma are reluctant or refuse to eat, so esophagostomy tubes are necessary. If the tube is not placed, soft food or gruel should be fed for 4 weeks. Under no circumstances ought the animal to chew on toys or other chewy objects.1,10,12,13 Moreover, antimicrobials against anaerobes (e.g. amoxicillin with clavulanic acid, metronidazole, clindamycin), and non- steroidal antinflammatory drugs should be administered.7,17 Opioids should be additionally prescribed if needed, depending on the surgical trauma, during the first postoperative hours or days. 17 Chlorexidine is also prescribed in order to reduce the microbial load of the oral cavity and the materials of osteosynthesis. Care should be taken to reduce the food remnants and plaque accumulation, especially when resin has been used.1,10,13
Delayed union and non-union represent the most common complications after mandibular reconstruction as a result of loose or fractured osteosynthesis materials, inappropriate technique or teeth affected by periodontitis in the fracture line. Malocclusion represents another common complication. In addition, intraosseous materials may cause tooth trauma, leading to their necrosis and abscessation. 1,3,10,22
Aim of the present study was to investigate the occurrence, causes, location, treatment and follow-up of fractures of the mandible in cats that were admitted at the Companion Animal Clinic of the Aristotle University of Thessaloniki during the period 2008- 2015.
> Materials and Methods
After retrieving medical records concerning the period 2008-2015, 23 cases of mandibular fractures in cats were enrolled. Some of the animals exhibited more than one fractures, resulting in 33 fractures to be studied. Incidence in relation to gender and age, as well as the cause and fracture type were studied. Furthermore, the accurate location of the fractures and the number of cases with multiple fractures and/or fractured teeth were investigated. The type of techniques which were applied and possible complications are being discussed. Finally, followups and postoperative course are mentioned. Postoperative course is classified as:
- unsuccessful, in case of non-union or malocclusion and difficulty in prehension and chewing of food.
- acceptable, when healing of the fracture site was accomplished with minimum malocclusion but no difficulty in prehension and chewing of food.
- excellent, when fracture healing and occlusion were ideal.
Statistical analysis was performed using IBM SPSS Statistics software.
> Results
 Incidence of fractures
Incidence of fractures
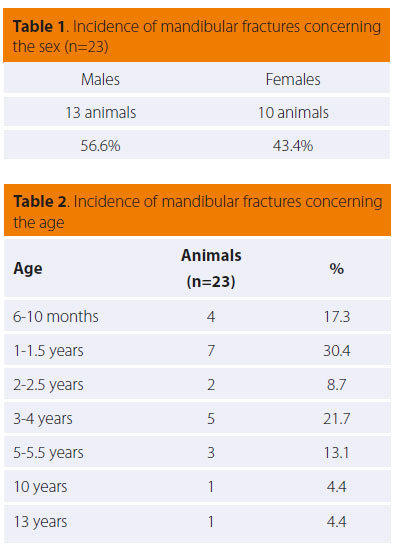
As shown in Table 1, fractures of the mandible were more common among male cats (13/23), even though results did not reach statistical significance. Table 2 shows that young cats are more prone to fractures (11/23 age≤ 1.5 years, 18/23 age ≤4 years), with a mean age of 3 years. The result was statistically significant (p< 0.05) in animals under the age of 4.
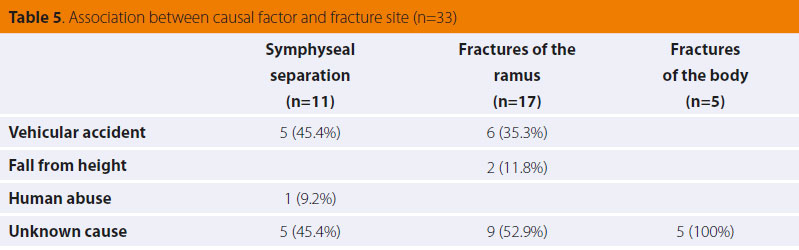
Cause
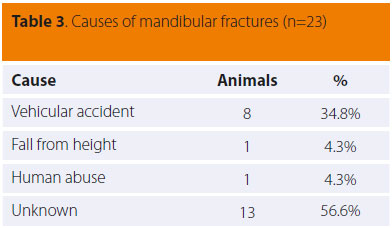
The most common cause of mandibular fracture was vehicular accidents (8/23), followed by fall from height and human abuse (1/23). However, a large number of cases (13/23) was of unknown cause, because the animals were found or returned home already injured (Table 3).
Location
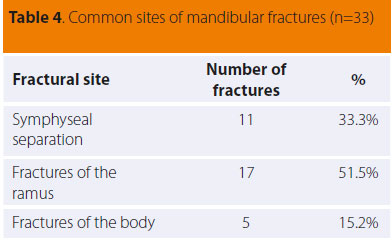
Twentythree cases involved 33 fractures of the mandible because four animals suffered from multiple fractures (2-4 fractures per case). Eleven cases involved the mandibular symphysis, five the body of the mandible and seventeen of them the ramus (condylar or subcondylar fractures) (Table 4). In 11 out of 17 fractures of the ramus, there was concurrent partial or complete ankylosis of the temporomandibular joint and inability to open the mouth because of an old fracture. In four cases, fractures of the ramus were bilateral. Concerning the fractures of the body, one was found in the incisor area, three in the premolar area and one was found near the left angular process. It should be noted that in 4 out of 23 cases, ten tooth fractures were noted. More specifically, six fractures concerned the canines, three the premolars and one the molar tooth. Table 5 illustrates the relation between the cause and the fracture site.
Treatment
Ten out of eleven separations of the symphysis were repaired using a circumferential orthopaedic wire just distal to the mandibular canines, while one case was treated with a wire in a figure-of-8 placed around the mandibular canines and was stabilised with acrylic resin.
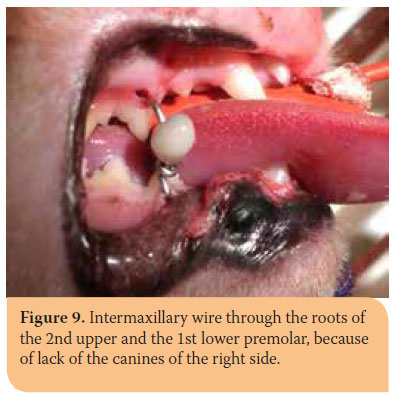 Diagnosis was confirmed soon after the causal factor in 6 out of 17 fractures of the ramus without signs of ankylosis of the temporomandibular joint (TMJ). In 5 of those 6 cases, bonding the upper and lower canines together with acrylic resin was performed. Canines of the right side were absent in the 6th fracture, so inter-maxillary fixation between the roots of the second upper and the first lower right premolar teeth and bonding of the left upper and lower canines was applied (Picture 9). In 11 out of 17 fractures of the ramus, diagnosis was set weeks later and partial or complete inability to open the mouth was detected. These 11 fractures pertained to 8 cats, in 5 of which the fracture was unilateral but was bilateral in 3. In 10 out of 11 cases condylectomy was inevitable due to fracture. In the eleventh case, the callous mechanically attempted to be destroyed by opening the mouth and then the canines were bonded together. However, soon after resin removal, the animal was unable to open its mouth and condylectomy was ultimately performed.
Diagnosis was confirmed soon after the causal factor in 6 out of 17 fractures of the ramus without signs of ankylosis of the temporomandibular joint (TMJ). In 5 of those 6 cases, bonding the upper and lower canines together with acrylic resin was performed. Canines of the right side were absent in the 6th fracture, so inter-maxillary fixation between the roots of the second upper and the first lower right premolar teeth and bonding of the left upper and lower canines was applied (Picture 9). In 11 out of 17 fractures of the ramus, diagnosis was set weeks later and partial or complete inability to open the mouth was detected. These 11 fractures pertained to 8 cats, in 5 of which the fracture was unilateral but was bilateral in 3. In 10 out of 11 cases condylectomy was inevitable due to fracture. In the eleventh case, the callous mechanically attempted to be destroyed by opening the mouth and then the canines were bonded together. However, soon after resin removal, the animal was unable to open its mouth and condylectomy was ultimately performed.
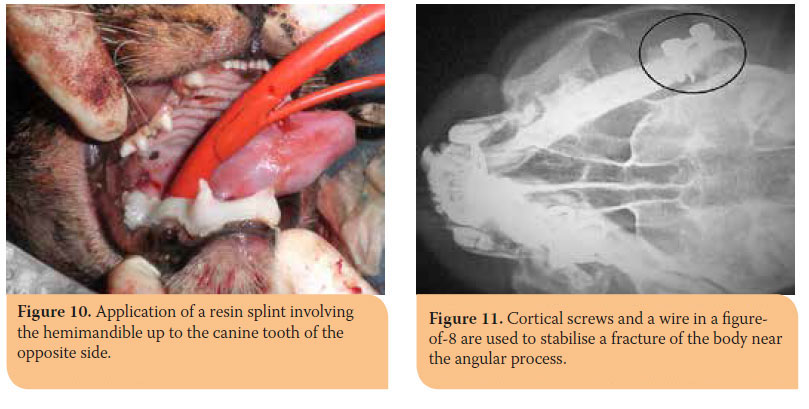
Concerning the fractures of the body of the mandible, 3 out of 5 which were located in the molar area were treated with interdental or/and intraosseous wiring and acrylic resin on the teeth. In particular, resin was applied on the whole hemimandible up to the canine of the same or the opposite mandible (Picture 10). In an oblique fracture of the left angular process, bone screws and a figure-of-8 wire were implanted (Picture 11) and intraosseous wiring was used in a fracture of the incisor area.
In three out of four cats with multiple fractures, upper and lower canines were bonded together to completely immobilise the jaws. Additionally, 9 out of 10 fractured teeth were extracted and one was temporarily sealed with resin. None of the aforementioned teeth was involved in the fracture line.
Supplementary action was taken in some cases to ensure better postoperative care. Specifically, tracheostomy was conducted in 8 out of 23 cases, because of ankylosis in 7 of them and extended sublingual edema in 1. Moreover, an esophagostomy tube was introduced in 5 cats.
Depending on the severity of the case, 18 out of 23 animals were hospitalised, even though it was proposed in all cases.
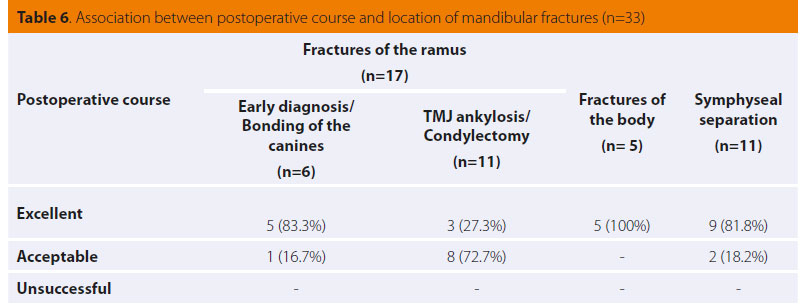
Post-operative course
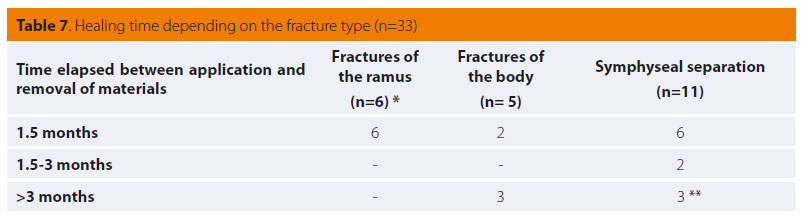
The outcome was excellent or acceptable in the majority of cases (Table 6). A statistically significant result between the two groups of mandibular fractures was found. Bonding of the canines provided a better outcome. Fracture healing was determined after radiographic examination and the time of materials removal is mentioned in Table 7. One animal required revision surgery and a couple of other animals were presented with minor complications, which did not require further actions. In particular, reversible gingivitis appeared in eight animals with acrylic resin on the teeth. In one case with fracture of the body, mobility of the resin splint was noticed, but the fracture healed leaving a mild malocclusion which did not interfere with food prehension and mastication.
Concerning the fractures of the ramus, one of the cases, where the canines were bonded together, failed, because of the initial attempt to destroy the already formed callus. Furthermore, in 2 out of 5 cats with unilateral condylectomy, mild displacement of the mandible towards the opposite side was noticed but the animals did not experience any discomfort.
In 2 out of 10 cases with sympyseal separations treated with cerclage wire, mild displacement of the mandible without traumatising the soft tissues was recorded. Moreover, dehiscence of the skin overlying the knot occurred in 2 cases with displacement of the knot in one of them. Both complications were attributed to late admission for removal of the materials. Finally, delayed healing of the symphysis was noticed in one case, which was resolved with delayed removal of the materials.
> Discussion
Fractures of the mandible in cats are quite common in clinical practice, especially after accidents.1-6 The number of cases reported here and the overall number of fractures in them seem to confirm this fact. It is interesting that the majority of the reported incidences resulted after trauma and none of them was pathological due to periodontitis or neoplasia. This fact may be associated with the mean age of the animals (three years). The results of this study indicate that young males are more prone to fractures of the mandible. According to Umphlet and Johnson (1988), young animals are bolder and risky. Moreover, they might be involved more commonly especially during reproductive periods. However, the results of the current study do not set a statistically significant difference between males and females. Concerning the age, it seems that young cats are prone to mandibular fractures. If cats up to the age of four are added to the list, the age groups (younger or older than four) are statistically significant.
According to the literature, symphyseal separations are the most common fracture types, especially after falling from heights.1,2,4-8 The latter is not confirmed in the current study. Even though the cause of fracture is unknown in 5 out of 11 cases, vehicular trauma is the most common cause. Every animal should be checked for separation of the symphysis after head trauma. Moreover, in contrast to other studies, fractures of the ramus were common (17 fractures of the ramus as opposed to 11 symphyseal and 5 fractures of the body). It is possible that a large number of cases were admitted for second opinion (14 out of 23, 61%). Symphyseal fractures can be treated easily, and they are often treated in first opinion practices, even though extra care should be taken to reestablish proper occlusion.
On the contrary, fractures of the ramus are more challenging. In cats, this type of fracture usually co-exists with other fractures of the maxilla and the mandible, especially with symphyseal separations.1,4,12,23 This was also found in the present study. Diagnosis of such fractures can be difficult and sometimes they are diagnosed either after TMJ ankylosis has occured or after sympheseal repair, when mallocclusion becomes evident. The well-developed muscles in the area of the ramus often do not allow identification of crepitus or abnormal movement. Sometimes, diagnosis is hard to be made even after radiography, because of the small size of the bones and superimposition of other structures.6,17,23 It is interesting that diagnosis was made only in 6 out of 17 fractures before TMJ ankylosis. Time of diagnosis affects treatment and outcome. The relevant table shows that jaw function is normal after bonding of the canines, whilst mild malocclusion was noticed after condylectomy. It seems that in case of head trauma, integrity of the ramus should be checked. It is obvious, that if diagnosis is set after TMJ ankylosis, condylectomy is required and restoration of normal function is not complete.
As it is also described in the literature, most cases of symphyseal separation were treated with a cerclage wire behind the canines.1,5,6,8,10,11 Normal occlusion of the canines should always be checked before the end of surgery because disarticulation of the mandible, fracture of the ramus or bone loss in the area of the symphysis may co-exist. In such cases, concurrent trauma should also be addressed and when bone loss is present, using wire in a figure-of-8 and acrylic resin on the canines is the preferred method.
Three out of five fractures of the body were treated with a combination of interdental or/and intraosseous wire and acrylic resin on the teeth. The outcome was completely successful in these cases. Fracture reconstruction with plates and screws or with intraosseous wire is quite difficult in cats because of the small size of the mandible. Difficulty pertains to avoiding injury of the roots or causing another fracture, especially if materials of inappropriate size are chosen. On the other hand, use of acrylic resin on the teeth allows for excellent stability, is minimally invasive and of low cost.3
Finally, extraction of teeth involved in the fracture line was not required in any of the animals. On the contrary, in many cases, these teeth were involved in the treatment plan.
> Complications
The only important complication was recorded in one case, where destruction of the already formed TMJ callus was attempted and the canines were bonded together. Soon after removing fixation materials, condylectomy was performed because of relapse. It seems that condylectomy is the treatment of choice, if TMJ ankylosis is evident.
Concerning the cases where a splint of resin on the teeth was applied, partial detachment was recorded twenty days later in one case. Even though the formed callus adequately stabilised the fracture, mild malocclusion was caused. Moreover, gingivitis was caused in all cases after removing the materials. Gingivitis is fully reversible and subsides within a few days after scaling and topical application of products containing chlorhexidine. Such products can contribute to milder forms of gingivitis, if they are used daily during treatment. Concerning the first complication, fixation materials should remain in place for one and a half months.
Finally, in some cases of unilateral condylectomy, mild shift of the mandible towards the opposite side was noticed. This complication did not cause any problem in prehension of food and mastication and no further actions were required.
> Conclusions
To sum up, fractures of the mandible in the cat should be treated only if no other life-threatening condition co-exists.
Even though some mandibular fractures seem easy to repair, managing them can be challenging. The mandible should be thoroughly checked for concurrent, less obvious fractures.
Apart from fracture healing, normal occlusion should also be assured.
Each fracture should be treated individually, depending on its location, type and the rest of the relevant parameters.
If the animal experiences difficulty in eating pre or postoperatively, care should be taken for adequate feeding.
> References
1. Jerram RM. Mandibular fractures and dislocations. In: Saunders Manual of Small Animal Practice. Birchard SJ, Sherding RG. 3rd edn. Mendor Editions S.A.: 2008, pp. 1037-1042.
2. Umphlet RC, Johnson AL. Mandibular fractures in the cat. A retrospactive study. Vet Surg 1988, 17: 333-335.
3. Bennet JW, Kapatkin AS, Marretta SM. Dental composite for the fixation of mandibular fractures and luxations in 11 cats and 6 dogs. Vet Surg 1994, 23: 190-194.
4. Smith MM, Kern DA. Skull trauma and mandibular fractures. Vet Clin North Am Sm Anim Prac 1995, 25: 1127-1148.
Papadimitriou SA. An update in mandibular fractrures treatment. 1st Conference Hellenic Association of Orthopaedic and Traumatology, 2004, Proceedings, pp. 12-19.
6. Moores AP. Feline skull fractures. Proceedings of the European Society of Veterinary Orthopaedics and Traumatology 2008-14th ESVOT Congress, Munich, Germany, pp. 160-162.
7. Matis U, Kostlin R. Symphyseal separation and fractures involving the incisive region. In: Oral and maxillofacial surgery in dogs and cats. Verstraete FJM, Lommer MJ (ed). 1stedn. Saunders-Elesevier: 2012, pp. 265-274.
8. Reiter AM, Lewis JR, Harvey CE. Dentistry for the surgeon. In: Veterinary surgery-small animal. Tobias KM, Johnston SA (ed). 1st edn. Saunders-Elesevier: St Louis, Missouri, 2012, pp. 1037-1053.
9. Boudrieau RJ, Verstraete FJM. Principles of maxillofacial trauma repair. In: Oral and maxillofacial surgery in κdogs and cats. Verstraete FJM, Lommer MJ (ed). 1stedn. Saunders-Elesevier: 2012, pp. 233-242.
10. Johnson AL. Management of specific fractures. In: Small Animal Surgery. Fossum TW, Dewey CW, Horn CV, et al (ed). 4rth edn. Elsevier- Mosby: St Louis, Missouri, 2013, pp.1106-1214.
11. Verstraete FJM. Maxillofacial fractures. In: Textbook of Small Animal Surgery. Slatter D (ed). 3rd edn. WB Saunders: Philadelphia, 2003, pp. 2190- 2207.
12. Lantz GC, Verstraete FJM. Fractures and luxations involving the temporomandibular joint. In: Oral and maxillofacial surgery in dogs and cats. Verstraete FJM, Lommer MJ (ed). 1st edn. Saunders-Elesevier: 2012, pp. 321-332.
13. Smith MM, Legendre FJ. Maxillofacial fracture repair using noninvasive techniques. In: Oral and maxillofacial surgery in dogs and cats. Verstraete FJM, Lommer MJ (ed). 1stedn. Saunders-Elesevier: 2012, pp. 275-284.
14. Harvey CE, Emily PP. Oral surgery. In: Small animal dentistry. Mosby– Year Book: Philadelphia, 1992, pp. 312–377.
15. Wiggs RB, Lobrise HB. Oral fracture repair. In: Veterinary dentistry: principles and practice. Lippincot-Reiven: Philadelphia, 1997, pp. 259-279.
16. Smith MM. Pharyngostomy endotracheal tube. J Vet Dent 2004, 21: 191-194.
17. Papadimitriou S. Mandibular fractures. University lectures. School of Veterinary Medicine, Aristotle University of Thessaloniki, Thessaloniki, 2014.
18. Legendre L. Intraoral acrylic splints for maxillofacial fracture repair. J Vet Dent 2003, 20: 70-78.
19. Niemec BA. Intraoral acrylic splint application. J Vet Dent 2003, 20: 123-125.
20. Boudrieau RJ. Maxillofacial fracture repair using intraosseous wires. In: Oral and maxillofacial surgery in dogs and cats. Verstraete FJM, Lommer MJ (ed). 1st edn. Saunders-Elesevier: 2012, pp.285-292.
21. Marretta SM. Maxillofacial fracture complications. In: Oral and maxillofacial surgery in dogs and cats. Verstraete FJM, Lommer MJ (ed). 1st edn. Saunders-Elesevier: 2012, pp. 333-341.
22. Thaller SR, Mabourakh S. Teeth located in the line of mandibular fracture. J Craniofac Surg 1994, 5: 16-19.
23. Ticer J, Spencer CP. Injury of the feline temporomandibular joint: radiographic signs. Vet Radiol 1978, 19: 146-156.



