> ABSTRACT
Tooth problems are very common among small animals. The veterinarian encounters them frequently, and quite often has to suggest tooth extraction. Periodontal disease and tooth fractures are the most common indication for extraction, while clotting defects or other pathological conditions which may endanger the animal’s life are contraindications. Appropriate pre-anaesthetic control and regional anaesthesia and analgesia should be considered before the extractions. The veterinarian should use proper instruments and pieces of equipment for such procedures. There are two basic extraction techniques: namely, the open and the closed technique. The choice of either technique will depend on several factors. The most usual complications after extraction are root fractures, massive post operative bleeding and soft tissue trauma. Postoperatively, the animal should receive the appropriate analgesics, antimicrobials, recommendations concerning the animal’s diet and home dental care.
> Introduction
Small animal owners express a growing interest concerning the prevention and treatment of oral diseases and pathological conditions of the oral cavity. Consequently, the veterinarian has to deal with dental problems which frequently entail several tooth extractions.
After appropriate training, a veterinarian could be able to undertake and treat dental cases which can constitute a substantial source of income for his practice.
> Anatomic Considerations
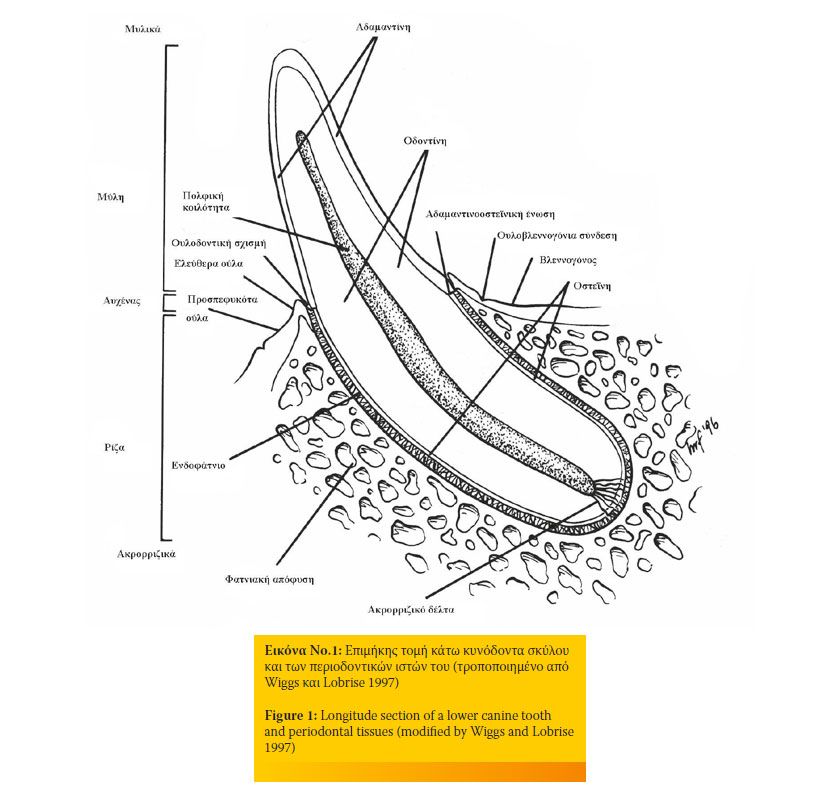
Figure 1 depicts the basic structure of a canine tooth and its periodontal tissues.
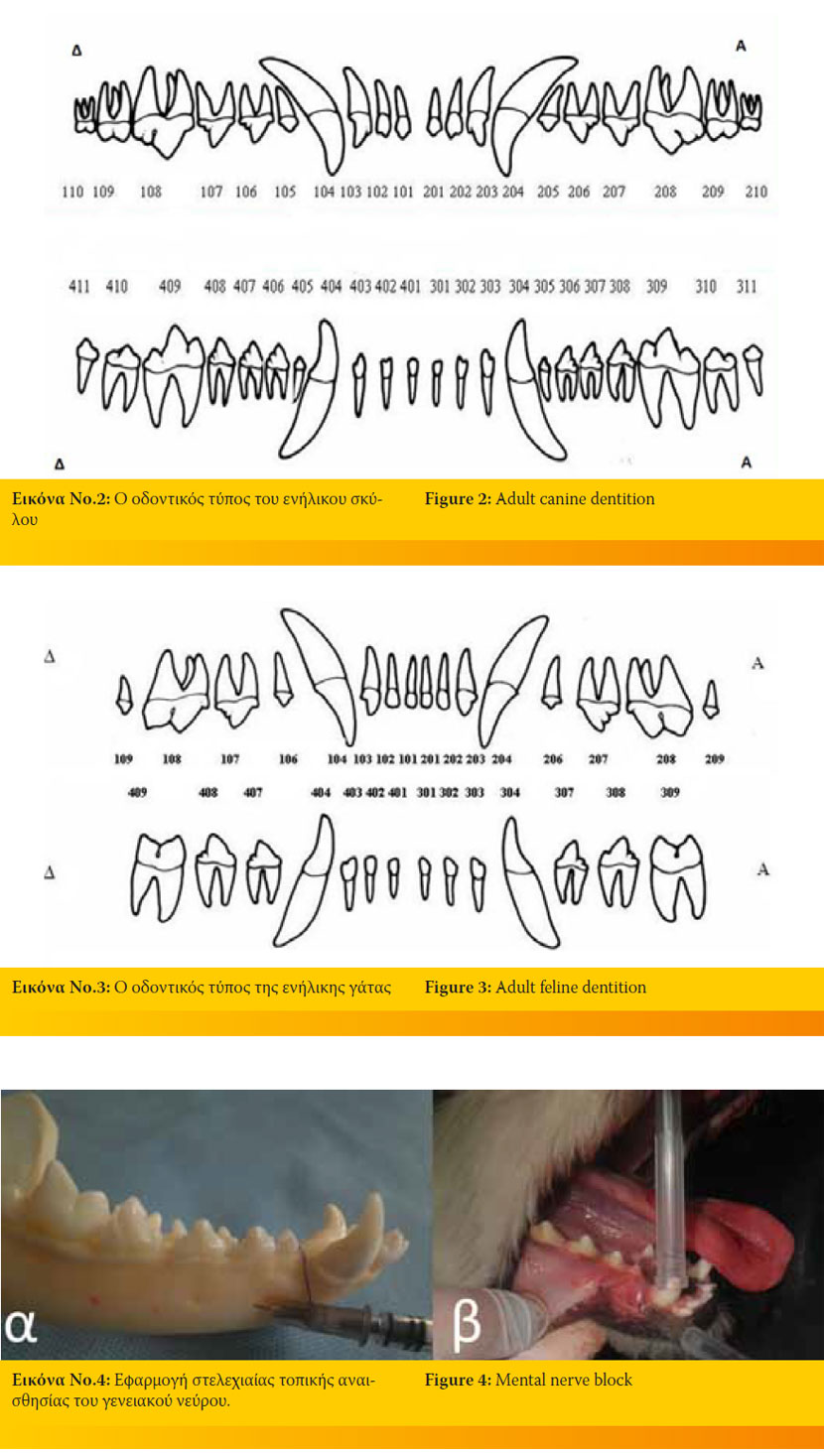
Figures 2 and 3 depict the number of roots to each tooth and the number of every tooth according to the modified triadan system (the first number represents the quadrant, with the maxillary right quadrant being 1. The individual teeth are represented by 2 digits with 01 being the first tooth from the midline and continuing distally along the arch to the last tooth, e.g. the upper first right incisor is 101 in dogs and cats, respectively). There are several differences concerning the number, the size and the shape between the two species. Because of their size and shape, cat teeth are far more fragile compared to dog teeth
> Indications for tooth extraction
Tooth extraction is one of the most common surgical interventions a veterinarian has to deal with. The indications of the procedure are the following:
1. Periodontal disease is the most common indication. Teeth are extracted in the following instances:
a) Periodontal destruction exceeds 50% of the length of the root. Loss of periodontal attachment is characterized by the creation of a periodontal sulcus and/or gingival recession.
b) tooth mobility exceeds 1mm
c) the tooth has been secondarily affected by endodontic disease
d) there is an oronasal fistula
e) the furcation in multi-rooted teeth is exposed. 1,2
2. Dental caries: tooth removal is performed mainly in dogs when most of the crown surface or the pulp is affected.2 Usually, the 1st and 2nd upper and lower molars are extracted. When the tooth destruction is not extended, the extraction is performed only if restoration or endodontic treatment are impossible.3
3. Tooth resorptions (mainly in cats): in 2nd, 3rd and 4th stage resorptions1 where the tooth is non-viable and painful.4
4. Feline chronic gingivostomatitis or stomatitis due to immunodeficiency: the microbial plaque and especially Gram (-) anaerobes are mainly responsible for the disease. Selective or full mouth tooth extractions are imperative. 5,6
5. Fractured teeth: absolute indications for tooth removal are oblique fractures involving the crown and the root.7 When the pulp is exposed, the tooth should either be endodontically treated or extracted.2
6. Teeth involved in a fracture line should only be removed if they are severely affected by periodontitis,3 if there is substantial motility, or the crown and root are severely fractured.5
7. Retained deciduous teeth: persistent primary teeth beyond the 7th month of age (usually deciduous canines) may interfere with the normal eruption of their permanent counterparts resulting in malocclusion and predisposing to periodontal disease of the permanent teeth. They should be removed as soon as possible.3,7
8. Impacted, embedded and non-functional bizarre looking teeth: impacted teeth are unerupted teeth covered by soft tissues and/ or bone. Embedded teeth have failed to fully erupt in their normal position. Impacted and embedded teeth should either be extracted if causing problems, or be monitored for infection, necrosis, odontogenic cyst formation or neoplastic transformation of the cyst.3
9. Supernumerary teeth: they predispose to early onset and deterioration of periodontal disease and orthodontic problems.3,6,7,8
10. Teeth causing malocclusion should be extracted, especially if other modalities of treatment have failed.6,8
11. In cases of a periapical lesion due to endodontic or periodontal disease. It is necessary to remove teeth that have caused abscesses or bone necrosis and osteomyelitis.3
12. Teeth involved in an oral tumour or an odontogenic cyst should be removed.3,8
13. Financial and subjective reasons that force the owners to elect extraction instead of other means of treatment.3,8,9,10,11
> Contraindications
As with every kind of surgery, animals experiencing other health problems, should not undergo tooth extractions.
Tooth extractions are contraindicated in animals with severe blood disorders3,7,9 such as clotting disorders and thrombocytopenia before they are properly treated. Moreover, they are not indicated in animals suffering from severe medical conditions like leukaemia and hypertension because wound healing would be delayed. They are also contraindicated in animals receiving specific nonsteroid anti-inflammatory drugs (e.g. aspirin), antineoplastic drugs, and generally every type of medication which might prolong bleeding time.3,9 Moreover, it is obvious that extractions cannot be performed in animals suffering from systemic diseases which render them unable to undergo general anaesthesia3,9 such as liver and kidney failure, severe hypertension, cardiac arrhythmias, respiratory disorders, etc. In addition, they should not be performed in animals receiving radiation therapy to the jaws.3,9 Finally, in cases of malignant neoplasms or haemangiomas of the jaw, tooth extractions might negatively affect prognosis.9
> Surgical procedure
Pre-surgical assessment
Before surgery, the surgeon should evaluate the overall condition of the oral cavity and each tooth individually as to whether the periodontium is healthy, the tooth is mobile and the crown integrity (massive destruction of the crown due to resorption may lead in tooth fracture during the procedure).12
Dental radiography (especially intraoral) is necessary in order to evaluate the morphology of the tooth and the pathology which renders its extraction necessary.7 It is important to predetermine the shape of the root, the proximity to other teeth and important structures and the quality of the underlying bone.12,13 In addition, radiographs will allow the surgeon to evaluate the malformation of the roots and possible ankylosis or resorption of the roots that might complicate the procedure. 3,13 Finally, dental radiographs form dental records which can be used in order to convince the owner about the necessity of dental care.15
In cases of concurrent pathological conditions, care should be taken in order to prevent infection, minimize bleeding, and avoid deterioration of the underlying condition.14 As previously mentioned, tooth extraction requires general anaesthesia, hence a full pre-anaesthetic blood and biochemical control is essential for the animal’s safety. Sick animals with unregulated metabolic disorders (e.g. unregulated diabetes mellitus, kidney failure, severe heart disease and clotting disorders) are not suitable candidates for general anaesthesia and major oral surgery. While dental procedures can improve quality of life, they should be postponed until the underlying pathological condition is under control.15,16
Analgesia, General and Regional Anaesthesia
Prevention of pain will help minimize anaesthetic requirements and postoperative pain and contribute to uneventful recovery. Multimodal analgesia helps to minimize the painful stimulation. Four main categories of medications are used: opioids, non-steroid anti-inflammatory drugs, α2-agonists and local anaesthetics.16,17,18,19,20,21
In particular, regional anaesthesia reduces the demand for deep general anaesthesia thus minimizing the demands of general anaesthesia and allowing quick recovery. As a rule, special local anaesthetics for dental use contain lidocaine and bupivacaine with or without epinephrine (for vasoconstriction). The main complications of local anaesthesia is the injury of a nerve, haematoma formation or the intravenous infusion of the drug. Using a small diameter needle and aspiration before infusion helps to minimize these risks.16,17,18,19,20,21,22,23
Depending on the region of the oral cavity the surgeon will operate, he can perform either regional or local anaesthesia. The most common sites are the following:5,16,17,18,19,20,21,22,23
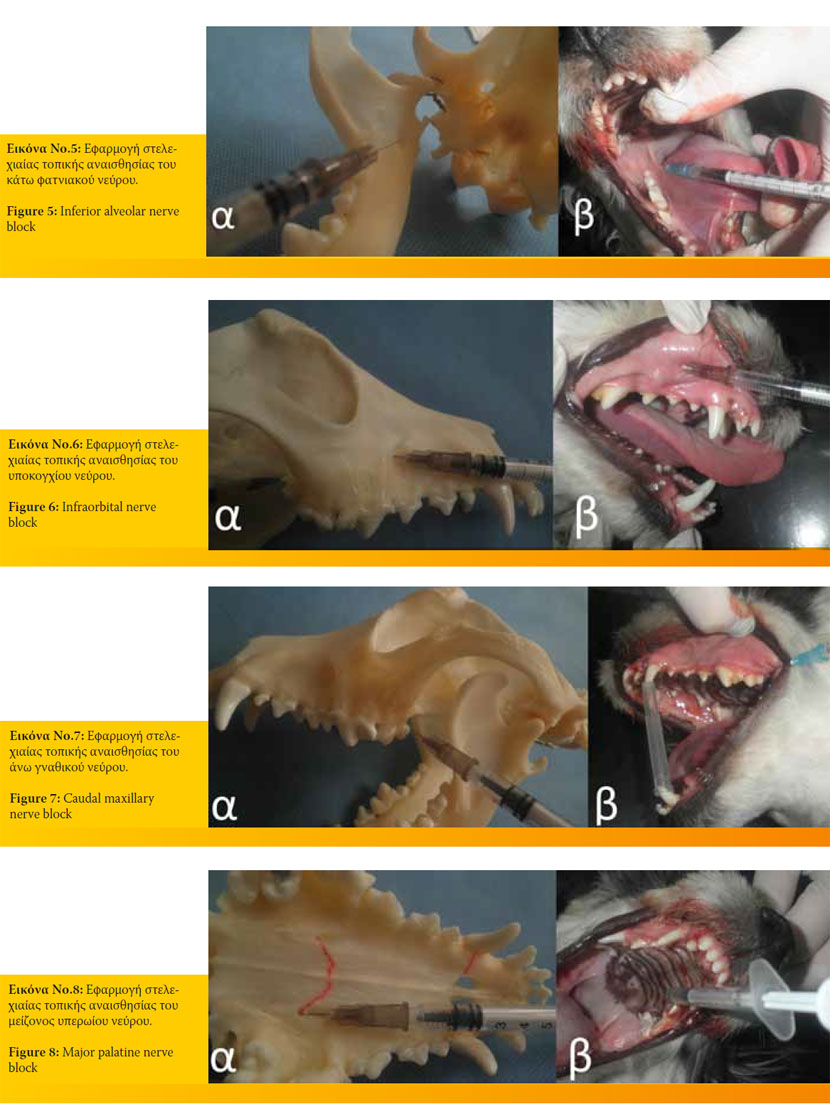
- Mental nerve block. It desensitizes the incisors, canines and the 1st-2nd premolars of the ipsilateral arch (Figure 4).
- Inferior alveolar nerve block. It desensitizes all the teeth of the arch. Its approach can be oral or extraoral (Figure 5).
- Infraorbital nerve block. It desensitizes the ipsilateral maxillary incisors, canine, premolars, and under circumstances, the modified technique can desensitize the first molar (Figure 6).
- Caudal maxillary nerve block. It may be approached intraorally or extraorally and desensitizes all the teeth of the quadrant (Figure 7).
- Major palatine nerve block. It can be approached intraorally by inserting the needle into the major palatine foramina. It desensitizes the ipsilateral 4th premolar and the two molars (Figure 8).
- Local anaesthetics can also be injected subperiostically, in the periodontal ligament, infrabony, into the pulp, in the furcation of each tooth.
Inhalation anaesthesia is commonly used in oral surgeries. The most commonly used anaesthetic agents are: halothane, isoflurane, sevoflurane, and desflurane.16,21 Even if the patient is anaesthesized with intravenous agents, he should be intubated with a properly inflated cuff to avoid aspiration of fluids, tartar and debris.3,5,13,16,19,21,24,25 Pharyngeal packs, such as gauzes or kitchen wipes (sutured together so that they can be later securely removed), should be placed in the pharynx in order to prevent aspiration of the aforementioned materials. The surgeon might also aspirate debris regularly during surgery with a suction device. One should keep in mind that the packing material must be removed before extubation.5,13,16,19,21,25 Placing an i.v. catheter is important for fluid and drug supplementation (antimicrobials, inotropics, vasoconstrictors) where necessary.16,21 The patient should be closely monitored during surgery (cardiological and respiratory function, colour of the mucus membranes, body temperature, etc.).16,20,21
Equipment
The basic dental equipment involves the following:
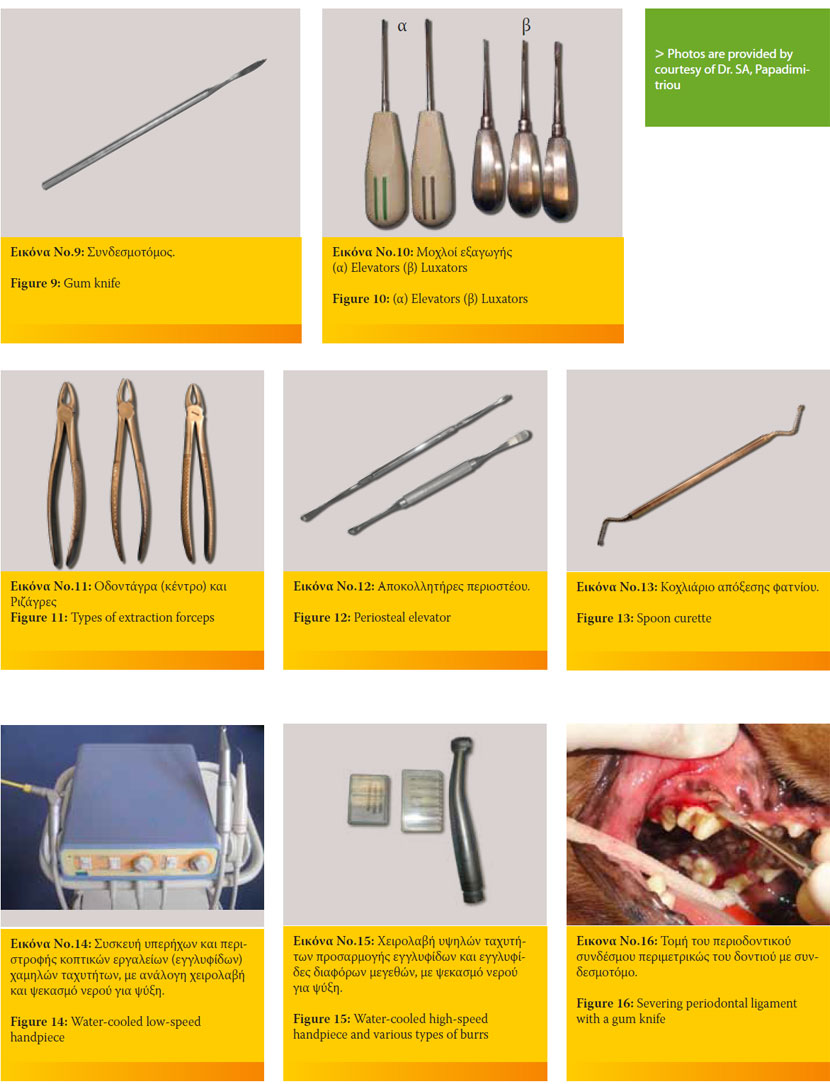
- Gum knife to severe the epithelial attachment and periodontal ligament (Figure 9).5
- Luxation instruments such as luxators (to severe the epithelial attachment and periodontal ligament) and elevators (used in a gentle rotational manner which causes rapture of the epithelial attachment and periodontal ligament). Luxators are finer and sharper instruments than the elevators, used at the beginning of the extraction before employing the elevators and the extraction forceps (Figure10).1,3,12,25,26,27
- Extraction forceps in various sizes and shapes used either for removing all sizes of teeth or broken apices (Figure 11).1,12,25,26,27,28
- Periosteal elevator to raise mucoperiosteal flaps from the alveolar bone during surgical extractions (Figure 12).25,26,28
- Curette for debriding and smoothening the alveolus after dislodging the tooth (Figure 13).28
- Low (30-35.000 rpm) (Figure 14) and high-speed water-cooled handpieces (300-400.000 rpm) compatible with various accessories (diamond and carbide burrs, diamond discs etc.) (Figure 15) for sectioning teeth and removing alveoral bone.5,25,26
> Principles and techniques of exodontics
Principles of exodontics
As in every surgery, extractions should conform to certain principles. It is important to be familiar with the anatomy of the oral cavity, the mandibles and the teeth to avoid iatrogenic trauma. Moreover, adequate lighting is necessary to see into the mouth.7,13,25,29
Water or a combination of air and water from a dental air-water syringe can be used to remove debris and air is used to dehumidify the area.7 Suction might be useful.13,19,29
The animal is positioned in lateral or dorsal recumbency2,12 to accommodate the surgeon.13,29,30 Gentle manipulations prevent iatrogenic trauma of the soft and hard tissues while allowing quick healing.2,13
Because of the special function of the oral cavity, it is not possible to perform aseptic surgeries. However, it is important to minimize the microbial burden. To do so, the surgeon may scale and polish the teeth and flush the oral cavity with a chlorhexidine solution.3,12,29,31 This practice will also prevent contamination of the alveolar process after the extraction, which will impede normal healing of the trauma.3 Preoperative administration of anaerobic-specific or broad spectrum antibiotics (amoxicillin-potassium clavulanate, clindamycin, metronidazole)31 are indicated for animals suffering from endocrinopathies, cardiological problems, severe topical or systemic pathological conditions or are debilitated or immunosuppressed, to prevent bacteraemia caused during dental surgeries.3,24,31 Antimicrobials should be in adequate concentration in the blood plasma during surgery. To achieve that, they must be administered intravenously as soon as the animal is anaesthetized.18
The veterinary surgeon should wear protective spectacles to minimize ocular exposure to aerolised micro-organisms and splatter, as well as debris12,20,25,29,30. Moreover, the operating room must be properly ventilated.25,29
Extraction techniques
Extractions can be performed using the closed technique (without raising a mucoperiosteal flap) or the open technique (raising a mucoperiosteal flap to expose the alveolar bone).3
In the closed technique, the surgeon levers the tooth and finally pulls it out by using the aforementioned equipment without having to remove alveolar bone.7 The technique is indicated for teeth with short apexes that are mobile due to periodontitis or trauma, having one root (incisors) or premolars previously sectioned.1,5
In the open technique, the surgeon has to raise a mucoperiosteal flap revealing the alveolar bone. Usually, the bone overlying the roots buccally is removed in order to enable removal of the tooth. The flap is then sutured in place to heal by 1st intention.7 This technique is suitable for extracting teeth with long apexes, such as the canines or the lower first molar, for multi-rooted teeth such as the upper 4th premolar and 1st molar, and generally for teeth strongly attached to their socket and when performing multiple extractions on the same quadrant.1,5
Choosing a technique over the other depends on the tooth’s morphology, the underlying pathology and the surgeon’s preference.7
The basic difference (in both techniques) regarding the single or multi-rooted teeth is the sectioning of the multi-rooted teeth with a highor low-speed handpiece. Accordingly, the root sections are removed as single-rooted teeth. It is important to identify the location of the furcation before completing the extraction.5
Closed technique:
Insert a gum knife or scalpel blade No 11 or 15 into the gingival sulcus and severe the periodontal ligament (Figure 16).
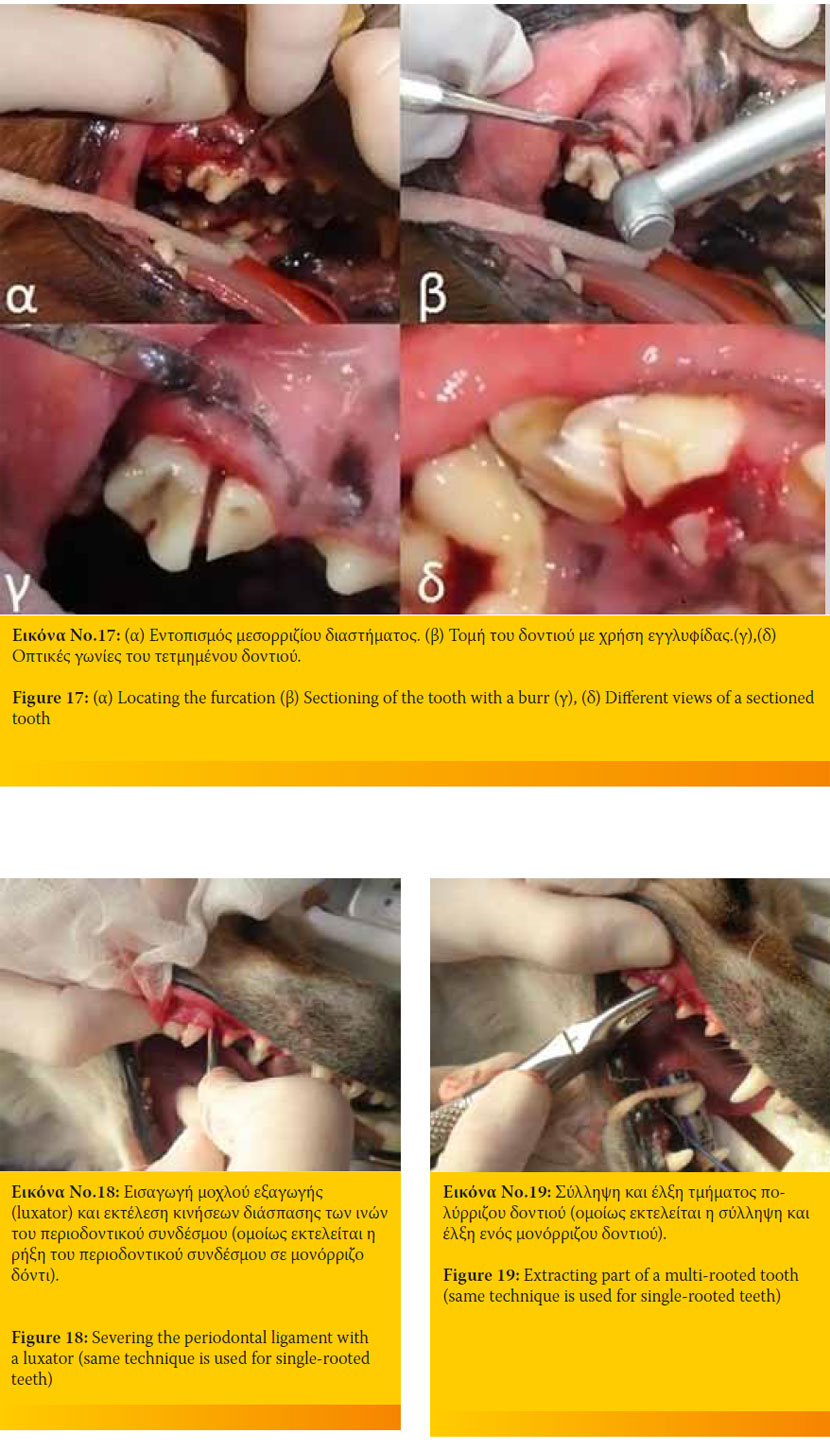
In cases of a multi-rooted tooth, reflect the gingiva to locate the furcation and section the tooth into single-rooted segments. Remove each segment as in a single-rooted extraction (Figure 17).
Force the luxator (if available) or elevator apically between the alveolar bone and root, using it as a wedge lever. Only the concave surface of the instruments should face the tooth and only the alveolar bone should be used as a wedge level, otherwise, the adjacent teeth may be traumatized or accidentally extracted.
The instruments are forced as apically as possible changing from smaller to larger sizes. Luxators are initially used, changing to elevators which can withstand greater amount of force without fracturing. The target of this process is to widen the periodontal space and severe the periodontal ligament to loosen the tooth and remove it (Figure 18).
Forceps are placed and the tooth is rotated slightly around its long axis with a steady pull and removed from its socket. If this proves difficult, the surgeon must not apply excessive force but should repeat the previous steps (Figure 19).
Trauma is left to heal by second intention. If necessary, debride the alveolus with a spoon curette or a proper size burr.
Open surgical technique
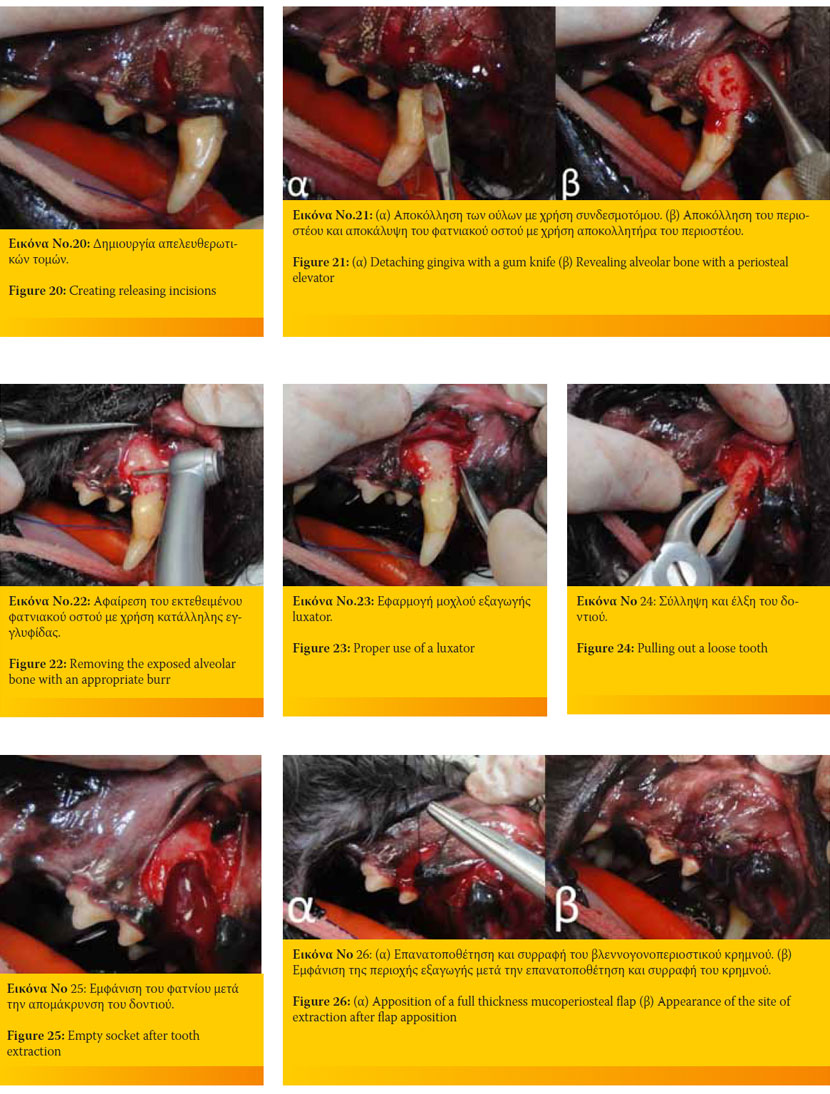
For the mucogingival flap, create releasing incisions on the buccal aspect of the gingiva with No 11 or 15 scalpel blades starting from the midpoint between adjacent teeth diverging apically (Figure 20).
Use a scalpel blade or sharp periosteal elevator to free the formerly incised attached gingiva from the underlying bone (Figure 21).
Remove the exposed alveolar bone with a lowspeed handpiece (in such a case, the area should be irrigated with tap water or normal saline) or a high-speed water-cooled handpiece. The bone area to be removed depends on the type of extraction (Figure 22).
In cases of a multi-rooted tooth, locate the furcation and section the roots as mention in the previous technique.
If necessary, slots can be burred at the mesial and distal aspects of the alveolar margin and the tooth to allow for the better elevator (or luxator if available) purchase (Figure 23).
Rotate and pull the loose tooth with extraction forces (Figure 24).
Proceed with lavage, debridement and alveoloplasty with spoon curette or low-speed handpiece with a proper burr of the extraction site (Figure 25).
Appose the flap carefully as it is important to the healing process (Figure 26).
Tooth extractions in cats are performed as previously described. However, the surgeon should keep in mind that the cat’s skull is smaller and more fragile than that of the dog.3,9,10 Moreover, cat teeth are smaller, more delicate and more fragile compared even to small-breed dogs.3,9 The surgeon should be more careful, his manipulations gentler and his instruments appropriate to avoid iatrogenic trauma in the area. In cases of multiple extractions, (such as in feline chronic gingivostomatitis) one should opt for open extractions.5
> Complications and their treatment
The most common complications and their treatment are listed below:
The most common complications and their treatment are listed below:
Root fracture: usually results after exerting a great deal of force to the elevator or extraction forceps.7 If the tooth being extracted has an inflamed pulp, periodontitis, osteolysis, fistula, abscess, etc., every part of the root must be removed to prevent further infection and inhibition of the healing process.3 If the part of the root is easily accessible, try to remove it with elevators or luxators and extraction forceps. If the part is nonaccessible, proceed to perform a mucoperiosteal flap and remove part of the buccal aspect of the alveolar bone with appropriate burr.5
Postoperative haemorrhage: excessive haemorrhage can pose a threat to the animal’s life.7 Blood may come from the bone or soft tissues. Haemorrhage can be controlled in four ways:
Apply gentle pressure or cold packs2,3
Place haemostatic sponge in the socket and suture the gums over.3,7,9,10
Electrocautery coagulation.2
Polygalactic acid which keeps the blood clot in the socket, improves healing and prevents postoperative osteitis.9,10
Oronasal communication: the communication between the oral and nasal cavities is caused due to periodontal disease, periapical disease, after tooth extraction in the upper incisor, canine or premolar area.2,3,7 Former loss or extraction of the upper canines is the most common cause of oronasal communication.2,3 A single or twolayer flap technique may be used to repair the communication.3
Fracture of the lower mandible: caused when excessive force is excreted during extraction or by unskillful technique.3 It occurs more often in small or medium size breeds or in cats during canine or first premolar extraction.3,7 Most of the times, the fracture needs to be surgically repaired.3
Local infection/osteomyelitis: a rare complication during extractions.9,10 Osteitis of the alveolus can sometimes develop into osteomyelitis.32 It happens when blood perfusion of the area is hampered or the extraction is extremely traumatic causing substantial damage of the periodontal tissues predisposing to bacterial infection.3,9,10 The infection is usually accompanied by a putrefying odour. It also causes great pain which can be treated with analgesics.32 Systemic antibiotics, necrotic tissue and alveolar bone debridement until bleeding is also recommended.2
Soft tissue trauma by opposing teeth: usually occurs in cats after a maxillary canine tooth is extracted. The upper lip contacts the lower canine and becomes traumatized. The lower canine can be treated with crown amputation or extraction.3
Iatrogenic trauma:
Bone thermal damage: caused by insufficient cooling of the burr when removing alveolar bone. Necrotic bone and soft tissues must be removed. Thermal damage can be avoided regardless of the type of handpiece used, when the burr is sufficiently cooled with tap water or saline irrigation.7
Soft tissue trauma: limited trauma of the adjacent gingiva is not important, though more extended trauma of the soft tissues results from excessive force applied during elevation and slippage of sharp instruments.3 If necessary, lacerated tissues can be sutured.
Trauma to adjacent tooth: great pressure during extraction can cause trauma or fracture of an adjacent tooth.3 If trauma is substantial, it should be reconstructed (with resin) or removed.5
Sublingual oedema and salivary mucocele: when manipulations are harsh3,7 or multiple extractions in the lower jaw are performed. If the oedema is severe, non-steroid anti-inflammatory drugs should be administered. Salivary mucocele (usually sublingual) is caused when the sublingualmandibular gland duct is traumatized during extraction.3 The sublingual mucocele may persist for several weeks before vanishing, otherwise it should be marsupializated or the complex sublingual- mandibular glands must be resected.5
Sublingual and subcutaneous emphysema: rarely caused after tooth sectioning or alveolar bone removal using high-speed equipment or from blowing air into the area.3,7 Soft tissue trauma should be sutured allowing the air to be absorbed. The animal should be closely monitored for signs of dyspnoea. Gentle manipulations prevent the creation of emphysema.3
> Postoperative care
Pain management
Analgesics should be pre- and postoperatively administered for 24-48 hours. Opioids and non-steroid anti-inflammatory analgesics are the treatment of choice.3,12,17,20,21,23,32,33 Regional anaesthesia helps to reduce postoperative pain.3,12,17,19,20,21,23,33
Oral and systemic hygiene
Maintaining good oral hygiene after tooth extractions contributes to quicker wound healing.12 Lowering the microbial load within the oral cavity is achieved by rinsing the mouth with a chlorhexidine solution preoperatively and by applying chlorhexidine gel or paste once or twice daily for two weeks postoperatively.3,5,12,14 The owner can also brush the teeth starting the 3rd-4th day after surgery, avoiding the extraction sites for a week.12 Antimicrobials should be used after due consideration because their irrational prescription can create resistant microbial species capable of initiating pathology in the future.10 Pre- and postoperative antibiotics are necessary in cases of immunosuppressive diseases (e.g. feline FIV, FeLV).33 Moreover, they should be given to animals suffering from cardiological problems or endocrinopathies when multiple extractions are performed, especially in cases of severe periodontal disease, or teeth responsible for periapical abscesses or fistulas.5,14 Clindamycin, metronidazole and amoxicillin and clavulanic acid are most commonly used.5,10
Diet
The animal should receive water as soon as it recovers from the general anaesthesia.3 Warm, soft food should be given for 7-10 days postoperatively, while dairy products should be avoided for 2-3 days.5 Chew toys are withheld while tissues heal.3,12 Most animals will eat and drink even after multiple extractions the first or second day after surgery.3,5 Force feeding or feeding tubes are rarely needed.3,12,33
> Postoperative management
The owner should monitor his pet for postoperative haemorrhage (blood tinted saliva is considered normal for two days post-operatively), pain, lethargy and anorexia, halitosis, and admit the animal for examination after 1-2 weeks to estimate the healing process.5,12,14,33 At that time, the veterinarian can inform the owner about the importance of home dental care, the prevention of oral diseases and the importance of tooth brushing.5,12,14
> References
1. Bellows J. Oral Surgical Equipment, Materials, and Techniques. In: Small Animal Dental Equipment, Materials and Techniques, A Primer. 1st edn. Blackwell Publishing: Oxford, UK, 2004, pp. 297-362.
2. Marreta SM, Tholen M. Extraction Techniques and Management of Associated Complications. In: Small Animal Oral Medicine and Surgery. Bojrab MJ, Tholen M (ed.). Lea and Febiger: Philadelphia, USA, 1990, pp. 75-94.
3. Reiter AM. Dental Surgical Procedures. In: BSAVA Manual of Canine and Feline Dentistry. Tutt C, Deeprose J, Crossley D (ed). 3rd edn. BSAVA: Quedgeley, UK, 2007, pp. 178-195.
4. Kesel LM. Assisting with Extractions. In: Veterinary Dentistry for the Small Animal Technician. 1st edn. Iowa State University Press: Ames, 2000, pp. 141-155.
5. Παπαδημητρίου Σ. Ενδείξεις και τεχνικές εξαγωγής δοντιών. Πανεπιστημιακές παραδόσεις 7ου εξαμήνου. Τμήμα Κτηνιατρικής Α.Π.Θ: Θεσσαλονίκη, 2014.
6. Tutt C. Exodontics. In: Small Animal Dentistry, A Manual of Techniques. Blackwell Publishing: Oxford, UK, 2006, pp. 131-171.
7. Gorrel C. Tooth Extraction. In: Veterinary Dentistry for the General Practitioner, 1st edn Saunders of Elsevier: Philadelphia, USA, 2004, pp. 157-174.
8. Holmstrom SE, Frost PF, Eisner ER. Exodontics. In: Veterinary Dental Techniques for the Small Animal Practitioner. 5th edn, Mosby Inc.: Philadelphia, 2007, pp. 291-338.
9. Harvey CE, Emily PP. Oral surgery. In: Small Animal Dentistry. Mosby-Year Book Inc.: St.Louis, 1993, pp. 312- 377.
10. Harvey CE. Basic Techniques-Extraction and Antibiotic Treatment. In: BSAVA Manual of Small Animal Dentistry. Harvey CE, Orr SH (ed). BSAVA: Cheltenham, 1990, pp. 29-35.
11. Holmstrom SE. Exodontics. In: Veterinary Dentistry, A Team Approach. 2nd edn. Elsevier Saunders: St. Louis, 2013, pp. 288-304.
12. Lommer MJ. Principles of Exodontics. In: Oral and Maxillofacial Surgery in Dogs and Cats. Verstraete FJM, Lommer MJ (ed). Saunders of Elsevier: Philadelphia, USA, 2012 pp. 97-114.
13. Holmstrom SE, Frost PF, Eisner ER. Exodontics. In: Veterinary Dental Techniques for the Small Animal Practitioner. 3rd edn. Saunders of Elsevier: Philadelphia, USA, 2004, pp. 291-338.
14. Lommer MJ, Verstraete FJM. Simple Extraction of Single-Rooted Teeth. In: Oral and Maxillofacial Surgery in Dogs and Cats.Verstraete FJM, Lommer MJ (ed). Saunders of Elsevier: Philadelphia, USA, 2012, pp. 115- 120.
15. Lommer MJ, Tsugawa AJ, Verstraete FJM. Extraction of Multirooted Teeth in Dogs. In: Oral and Maxillofacial Surgery in Dogs and Cats. Verstraete FJM, Lommer MJ (ed). Saunders of Elsevier: Philadelphia, USA, 2012, pp. 131-139.
16. Joubert K, Tutt C. Anaesthesia and Analgesia. In: BSAVA, Manual of Canine and Feline Dentistry. Tutt C, Deeprose J, Crossley D (ed). 3rd edn. BSAVA: Quedgeley, UK, 2007, pp. 41-55.
17. Tutt C. Pain Management. In: Small Animal Dentistry, A Manual of Techniques, Blackwell Publishing: Oxford, UK, 2006, pp. 229-238.
18. Kesel LM. Anesthesia, Analgesia and Postsurgical Support. In: Veterinary Dentistry for the Small Animal Technician. 1st edn. Iowa State University Press: Ames, 2000, pp. 101-120.
19. Gorrel C. Anesthesia and Analgesia. In: Veterinary Dentistry for the General Practitioner. Saunders of Elsevier: Philadelphia, USA, 2004, pp. 11-22.
20. Holmstrom SE, Frost PF, Eisner ER. Anesthesia and Pain Management in Dental and Oral Procedures. In: Veterinary Dental Techniques for the Small Animal Practitioner. 3rd edn. Saunders of Elsevier: Philadelphia, USA, 2004, pp. 601-624.
21. Pascoe PJ. Anesthesia and Pain Management. In: Oral and Maxillofacial Surgery in Dogs and Cats. Verstraete FJM, Lommer MJ (ed), Saunders of Elsevier: Philadelphia, USA, 2012, pp. 23-42.
22. Holmstrom SE. Local Anesthesia. In: Veterinary Dentistry, A Team Approach. 2nd edn. Saunders of Elsevier: St. Louis, 2013, pp. 135-149.
23. Bellows J. Local and Regional Anesthesia and Pain Control. In: Small Animal Dental Equipment, Materials and Techniques. A Primer. 1st Edn. Blackwell Publishing: Oxford, UK, 2004, pp. 105-114.
24. Holmstrom SE. The Complete Prophy. In: Veterinary Dentistry, A Team Approach. 2nd edn. Saunders of Elsevier: St. Louis, 2013, pp. 167-193.
25. Gorrel C. Equipment and Instrumentation. In: Veterinary Dentistry for the General Practitioner, 1st edn. Saunders of Elsevier: Philadelphia, USA, 2004, pp. 1-10.
26. Robinson J. Dental Instrumentation and Equipment. In: BSAVA, Manual of Canine and Feline Dentistry. Tutt C, Deeprose J, Crossley D (ed). 3rd edn. BSAVA: Quedgeley, UK, 2007, pp. 67-76.Holmstrom SE, Frost PF, Eisner ER. Dental Equipment and Care. In: Veterinary Dental Techniques for the Small Animal Practitioner. 3rd edn. Saunders of Elsevier: Philadelphia, USA, 2004, pp. 39-130.
27. Marreta SM (απόδοση στην ελληνική γλώσσα: Παπαδημητρίου ΣΑ, Ράλλης Τ). Οδοντιατρική και πα- θήσεις της στοματικής κοιλότητας και του φάρυγγα. In: Saunders Εγχειρίδιο Κτηνιατρικής των Μικρών Ζώων. 3rd edn. Mendor Editions S.A.: 2008, pp. 609-635.
28. Deeprose J. Operator Safety and Health Considerations. In: BSAVA Manual of Canine and Feline Dentistry. Tutt C, Deeprose J, Crossley D (ed). 3rd edn. BSAVA: Quedgeley, UK, 2007, pp. 56-66.Holmstrom SE, Holmstrom LA. Personal Safety and Ergonomics. In: Veterinary Dentistry, A Team Approach. 2nd edn. Saunders of Elsevier: St. Louis, 2013, pp. 117-134.
29. Gorrel C. Antibiotics and Antiseptics. In: Veterinary Dentistry for the General Practitioner, 1st edn. Saunders: Philadelphia, USA, 2004, pp. 23-28.
30. Crossley DA, notes for the British Veterinary Dental Association’s (BVDA), Basic Dentistry Courses, 2003.
31. Lommer MJ. Special Considerations in Feline Exodontics. In: Oral and Maxillofacial Surgery in Dogs and Cats. Verstraete FJM, Lommer MJ (ed). Saunders of Elsevier: Philadelphia, USA, 2012, pp. 141-152.