> Abstract
A 9-year-old male mixed breed dog was admitted for the management of a partial and full thickness thermal burn that was covering 45% of his body including the dorsal, lateral and ventral thorax and abdomen, medial thigh and caudal elbow. Medical honey (L-Mesitran® soft) was applied to the burn area on a daily basis and dressed with absorbent pads resulting in complete healing by contraction and epithelialisation 35 days after initial admission. Medical honey may be used as an effective alternative for the treatment of extensive skin burns.
> Introduction
Thermal burn injuries are rarely encountered in small animal practice. Tissue exposure to extreme temperatures usually results in cellular destruction ensuing in local or systemic effects.1 Thermal burns may be the result of accidental or deliberate exposure to flames or fire, scalds from hot liquids or gases, or from contact with a hot surface.2 Classification of burning injuries depends on the skin surface area that is affected and also on the depth of tissue destruction (superficial, partial thickness or full thickness burns).1,2 Burn depth serves as a critical prognostic indicator; superficial or partial thickness burns may heal without surgical intervention, but full thickness burns require either surgical reconstruction or secondary healing by contraction and epithelialization depending on the extent of the surface area involved.2 Honey has been used for the treatment of human wounds since ancient times with favourable outcomes. The healing properties of honey are due to its antibacterial action due to the hydrogen peroxide production that ensues after contact of honey with wound exudate, flavonoids and high sugar content that result in hyperosmosis eventually leading to bacterial dehydration, death and hyperacidity.3,4 Other properties of honey include anti-inflammatory and deodorising effects, debriding action and acceleration of tissue growth and granulation tissue formation.3-6 Natural honey may contain Bacillus spp and Clostridium spp and must not be used for medical purposes. Sterile, radiated honey that is derived from specific
pathogen-free hives is recommended for medical use.6,7 Manuka honey and Medihoney® are the types of honey most commonly used in clinical practice in humans. More recently, another medical product consisting of 40% irradiated honey, known as L-Mesitran®, was introduced to human medicine.8-10 Medical honey has also been recently introduced to veterinary medicine.5,6,11-14 There is, however, a paucity of scientific documentation concerning the wound healing effects of medical honey in veterinary medicine and only a few studies conducted in equines have shown promising results.13,14 The purpose of the present study was to evaluate the therapeutic effect of medical honey in second intention healing of an extensive partial and full-thickness skin burn in a dog and possibly to suggest an alternative therapy to the classic ointments and/or wound dressings.

> Case report
A 9-year-old male mixed breed dog was referred because of an extensive truncal thermal skin burn. The referring veterinarian, after performing an aggressive debridement of the necrotic tissue, had cleaned the wounded area thoroughly for the past six days, once daily, with chlorhexidine solution and applied a silver sulfathiazine cream topically. Additionally, the dog was treated with intravenous fluids and electrolytes, antibiotics and analgesics. On the day of admission, the dog was diagnosed with partial and full thickness burns affecting 45% of his body as estimated by calculation of the total body surface area.1 A few necrotic areas were evident on the dorsal thorax and granulation tissue extended to the dorsal, lateral and ventral thorax and abdomen, medial thigh and caudal elbow. Under general isoflurane anaesthesia, the wounded area was further debrided to remove the necrotic skin over the thorax, lavaged with normal saline, and dressed with non-adherent pads (Figures 1 and 2).

After 24 hours, and following lavage with normal saline, LMesitran soft (Triticum, Netherlands) was applied topically with a sterile gloved hand once daily and the wound was dressed with absorbent dressings (Zetuvit E, Hartman Germany) and bandages (Figure 3). Healthy granulation tissue appeared within 72 hours. L- Mesitran was applied daily following lavage of the burn area. For the first three days, bandage changes were performed under propofol anaesthesia. Thereafter, since L-Mesitran application was accompanied by discomfort, tramadol was administered for pain relief at a dose of 3 mg/kg im TID (Tramal, Vianex Greece) along with carprofen (Rymadil, Zoetis Greece) at a dose of 2 mg/kg bid per os. Epithelialization of the wound was evident five days after initial admission (Figures 4 a and b).


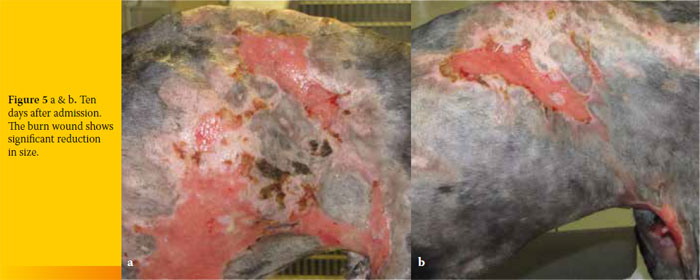
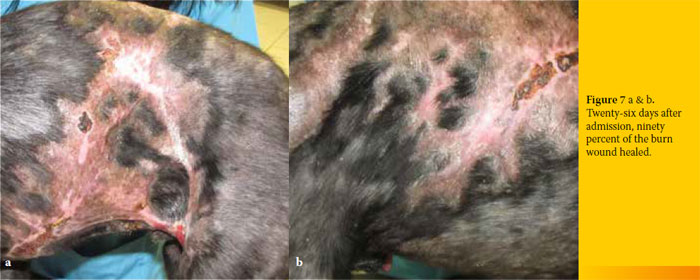
Ten days after admission, contraction of the wound was significant (Figures 5 a and b). On day 15, the epithelium had covered 50% of the burn area and on day 20, 75% of the burn healed (Figures 6 a and b). On day 26, the dog was discharged as 90% of the burn had healed, and contraction and epithelialization were sufficient (Figures 7 a and b). Small areas around the cranial thighs were still not healed and the owner was advised to apply mupirocin calcium ointment (Bactroban ointment, GlaxoSmithKline, Greece) topically, twice daily, until healing was complete. On re-examination 35 days after initial admission, the burn had healed completely (Figure 8). One year later, the dog is doing well.


> Discussion
In the case reported herein, the extensive burn was addressed initially at the time of admission with surgical debridement of residual devitalized tissue to avoid secondary infection and sepsis.1 This approach allowed for a shift from the inflammatory to the proliferative phase of wound healing, creating a healthy granulation tissue bed.1,2 In this case, due to the extensive area of the burn wound and the difficulty to pursue surgical reconstruction using flaps or grafts, we opted for a conservative approach using local application of medical honey that has shown promising therapeutic results for the healing of wounds and burns in humans, equines and dogs.3,5,11,13,14,15 L-Mesitransoft appeared to be a good alternative for the management of burn wounds in vivo and in vitro in humans.8,10 Manuka honey has been also found to minimize the wound area by decreasing retraction and overall to reduce healing time compared to controls, when applied on experimental equine wounds located on the limbs.13,14 L-Mesitran soft was reported to accelerate healing time and provide more re-epithelialization when compared to povidone iodine ointment and silver sulphadiazine cream that were applied to human burns and in vitro burn wounds, respectively.8,10,16 The outcome of this dog supports the findings in equines, and we found that L-Mesitran soft seems to help in speeding up the healing process by increasing granulation tissue formation time and reducing wound contraction and epithelialization time. As a result, the wound healed almost entirely within 26 days. Partial-thickness burns usually heal within 2-3 weeks whereas full- thickness burns take longer to heal.2 In the present case, the burn was partial and full-thickness and healed almost completely within the apparently short period of 26 days with no complications in terms of wound contracture involving the limbs.2 Application of L-Mesitran soft directly to the skin is followed by immediate coverage with absorbent bandages to avoid run-off from the burn surface.12 In this study, when L-Mesitran soft was applied to the burn, the dog seemed to be in discomfort due to pain. Pain was controlled by administering opioids and non-steroidal anti-inflammatory drugs. The exact cause of honey-related pain remains unclear and may be associated with hyperalgesia due to the burn injury and not to the honey itself or to the irritation of the tissues during removal of the honey-soaked dressings.3,5,17
In the present case, systemic antimicrobials were given empirically by the referring veterinarian on presentation. However, systemic antimicrobial therapy in the burn patient should only be administered in the presence of sepsis. On referral to the authors’ clinic, no systemic antibiotics were given throughout the whole treatment period since no signs of sepsis were present and so as to prevent the development of resistant microorganisms. In addition, in the presence of granulation tissue any antibiotics should be discontinued.
Mupirocin ointment should not be used or used sparingly in dogs and only following culture and sensitivity testing as resistance to methicilin-resistant Staphylococcus is increasingly reported in both humans and animals.18
One year after admission, the dog showed no restriction of movement or any other complications related to healing.
In conclusion, L-mesitran soft may provide an alternative to more expensive topical or systemic wound medications for the management of extensive burns. L-Mesitran soft seems to aid in speeding up granulation tissue formation and reducing second intention healing time in dogs with extensive thermal skin burns.
> References
1. Bohling MW. Burns. In: Veterinary Surgery Small Animal. Tobias KM, Johnston SA (eds). Elsevier: St Louis, 2014, pp. 1291- 1302.
2. Pavletic M, Trout NJ. Bullet, bite, and burn wounds in dogs and cats. Vet Clin Small Anim Pract 2006, 36: 871-893.
3. Vandamme L, Heyneman A, Hoeksema H, Verbelen J, Monstrey S. Honey in modern wound care: a systematic approach. Burns 2013, 39: 1514-1525.
4. Molan PC. The role of honey in the management of wounds. J Wound Care 1999, 8: 415-418.
5. Mathews KA, Binnington AG. Wound Management using honey. Comp Contin Educ Pract Vet 2002, 24: 53-60.
6. Overgaauw PAM, Kirpensteijn J. Application of honey in the treatment of skin wounds. Eur J Com Anim Pract 2006, 16: 1-3.
7. Postmes T, van den Bogaard AE. Honey for wounds, ulcers, and skin graft preservation. Lancet 1993, 342: 756-757.
8. Vandeputte J, van Waeyenberge PH. Clinical evaluation of L- Mesitran- a honey- based wound ointment. Prof Nurs Today 2007, 11: 26-31.
9. Morris C. The use of honey in wound care and the mesitran product range. Wounds 2008, 4: 84-87.
10. Boekema BKHL, Pool L, Ulrich MMW. The effect of a honey based gel and sulphadiazine on bacterial infections of in vitro burn wounds. Burns 2013, 39: 754-759.
11. De Rooster H, Declercq J. Honey for wound care: myth or science? Part 2: clinical cases with dogs. Flemish Vet Mag, 2008, 78: 75-80.
12. De Rooster H, Declercq J, van den Bogaert M. Honey for wound care: myth or science? Part 1: literature overview. Flemish Vet Mag, 2008, 78: 68-74.
13. Bischofberger AS, Dart CM, Parkins NR, Dart AJ. A preliminary study on the effect of manuka honey on secondintention healing of contaminated wounds on the distal aspect of the forelimbs of horses. Vet Surg 2011, 40: 898-902.
14. Bischofberger AS, Dart CM, Parkins NR, Kelly A, Jeffcot L, Dart AJ. The effect of short- and long- term treatment with manuka honey on second intention healing of contaminated and noncontamonated wounds on the distal aspect of the forelimbs in horses. Vet Surg 2013, 42: 154-160.
15. Potokar T. Antibacterial effect of medical honey L-Mesistran and its effect on wound healing. L- Mesitran Clinical data file 2014: 1-5.
16. Malik KI, Malik MA, Aslam A. Honey compared with silver sulphadiazine in the treatment of superficial partial-thickness burns. Int Wound J 2010, 17: 413-417.
17. Davidson JR. Current concepts in wound management and wound healing products. Vet Clin Small Anim 2015, 45: 537-564.
18. Loeffler A, Linek M, Moodley A, Guardabassi L, Sung JM, Winkler M, Weiss R, Lloyd DH. First report of multiresistant, mecA‐positive Staphylococcus intermedius in Europe: 12 cases from a veterinary dermatology referral clinic in Germany. Vet Derm 2007, 18: 412-421.



